All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Jennifer Jeung, University of Florida (USA), for contributing this case.


July 11-15, 2011
The Snow King Resort
Jackson, Wyoming (USA)
The 28th Annual Summer Update
in Clinical Immunology, Microbiology
and Infectious Disease
Course Topics:
This 24-hour review and update is intended to improve knowledge about the pathogenesis and clinical manifestations of infectious diseases, immunological mechanisms of disease and disease prevention, appropriate approaches to the diagnosis of infections and immunologic disorders, and utilization of the clinical microbiology and immunology laboratory including selection and interpretation of results.
This course will provide a forum for the exchange of ideas dealing with microbial infections as well as immunity to infectious diseases and immunologic disorders. Faculty consists of clinicians involved in patient care, pathologists, and clinical laboratory scientists. Discussion of timely topics by faculty and participants assures that this course will be informative, interesting, and relevant.
Course Directors:
Harry R. Hill MD, Larry G. Reimer MD, July Daly PhD
This course is approved for 24 AMA PRA Category I Credit(s)
Website
Schedule
Hotel
Register
[#2506]
(1) Thanks to Nikhil Sangle, M.D., University of Utah and ARUP Laboratories, for reviewing the entire B cell lymphoma chapter. We will be adding more images to this chapter over the next 1-2 months.
(2) We are always looking for reviewers of our chapters, or parts of chapters. If interested, email us your CV and the chapters / topics you are interested in reviewing. More information about reviewing is found here.
Visit and follow our Blog to see recent updates to the website.
Case #204
Clinical history:
A 60 year old Caucasian man had an incidental 5 cm solid left lower pole renal mass on computed tomography (CT) scan. There was no evidence of metastatic disease or masses elsewhere on abdominal and chest CT scans. The patient underwent a left radical nephrectomy, and a tan, soft, well encapsulated mass 4.0 x 4.0 x 3.0 cm was present in the lower pole. No renal vein involvement was identified. Microscopically, the tumor invaded through the capsule with extension into the perinephric and pericalyceal adipose tissue and was pathologic stage pT3 pNX.
Gross images:
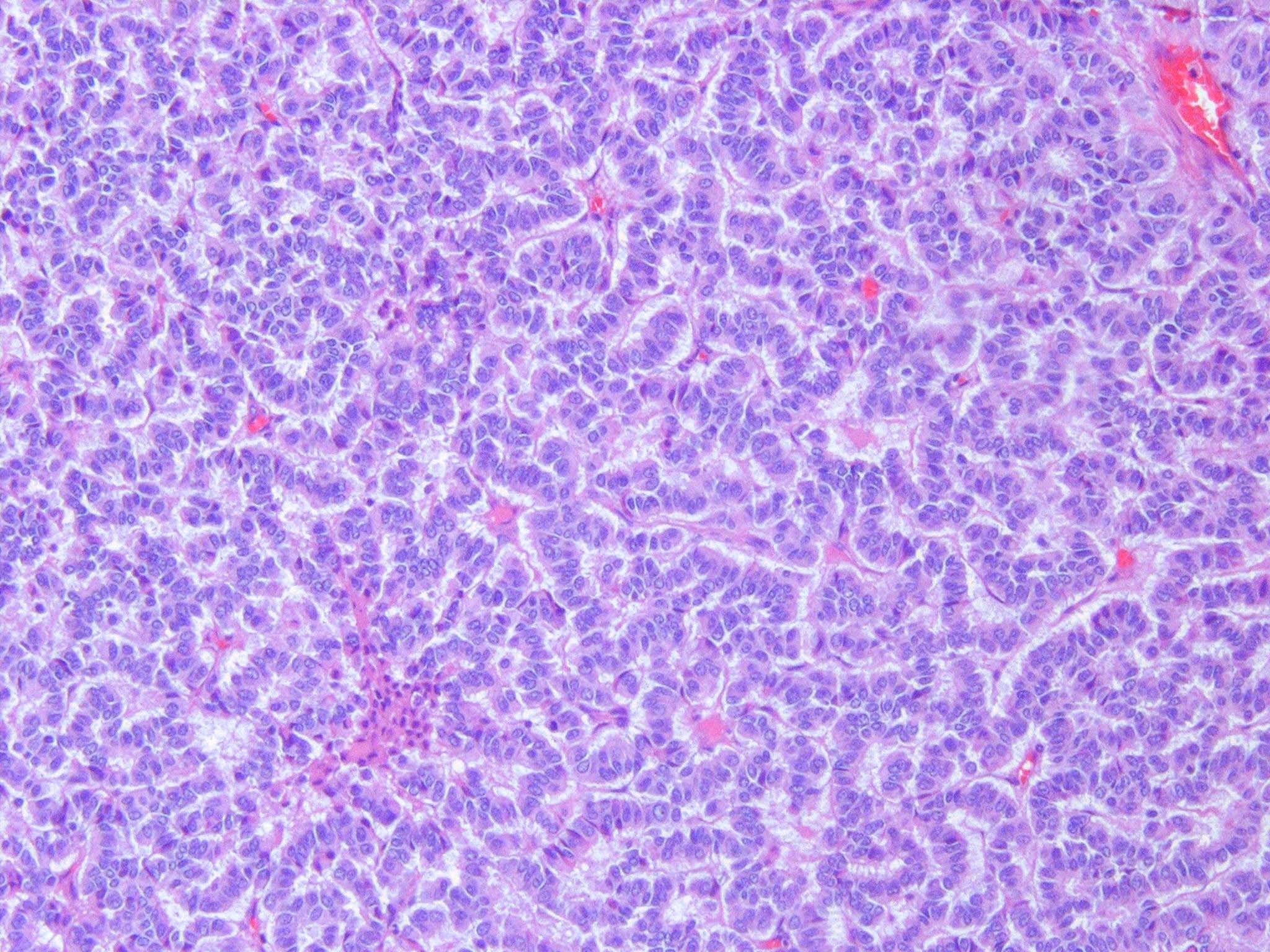
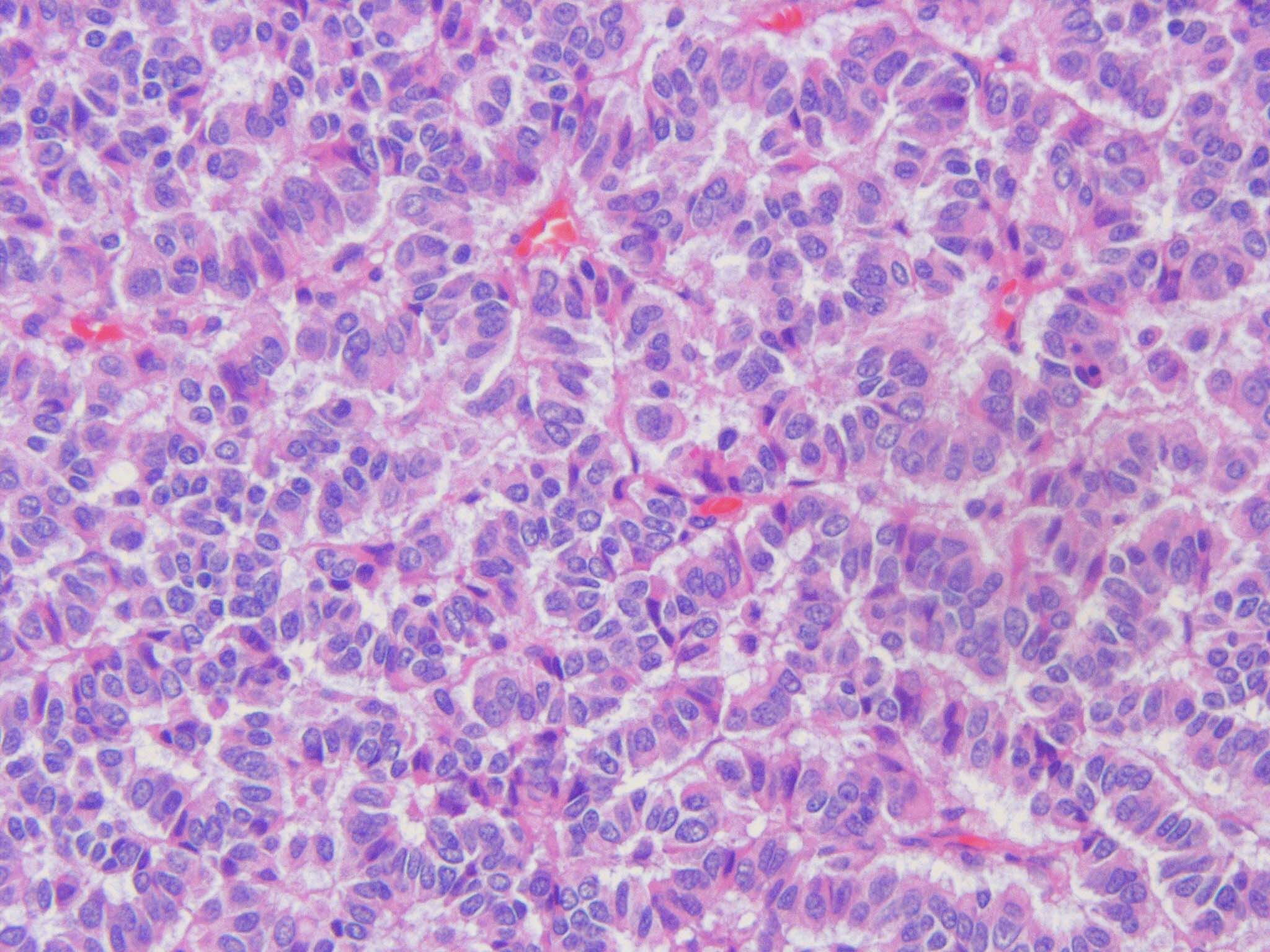
Microscopic images:
What is your diagnosis?
Diagnosis: Primary renal well differentiated neuroendocrine tumor (carcinoid)
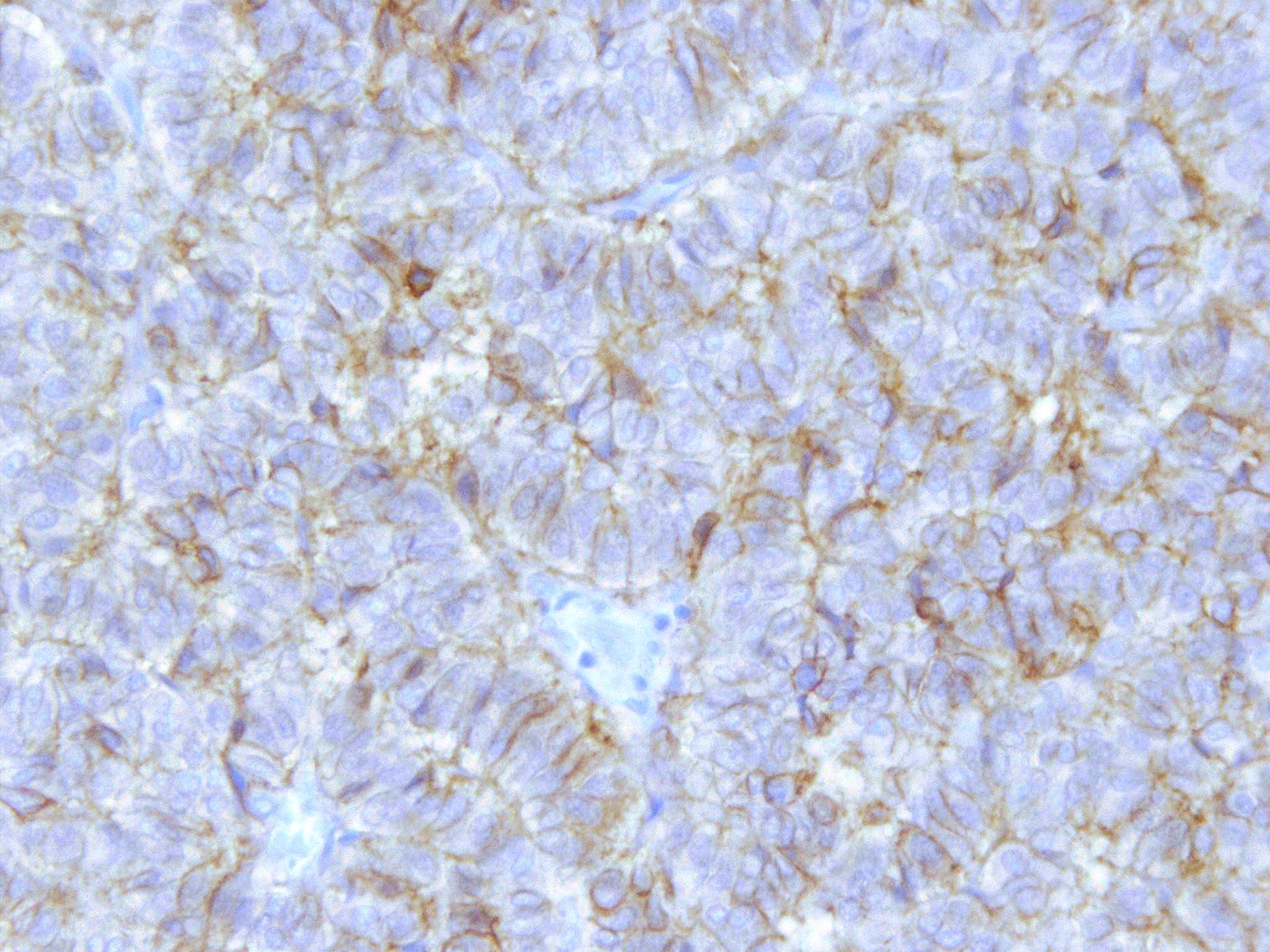
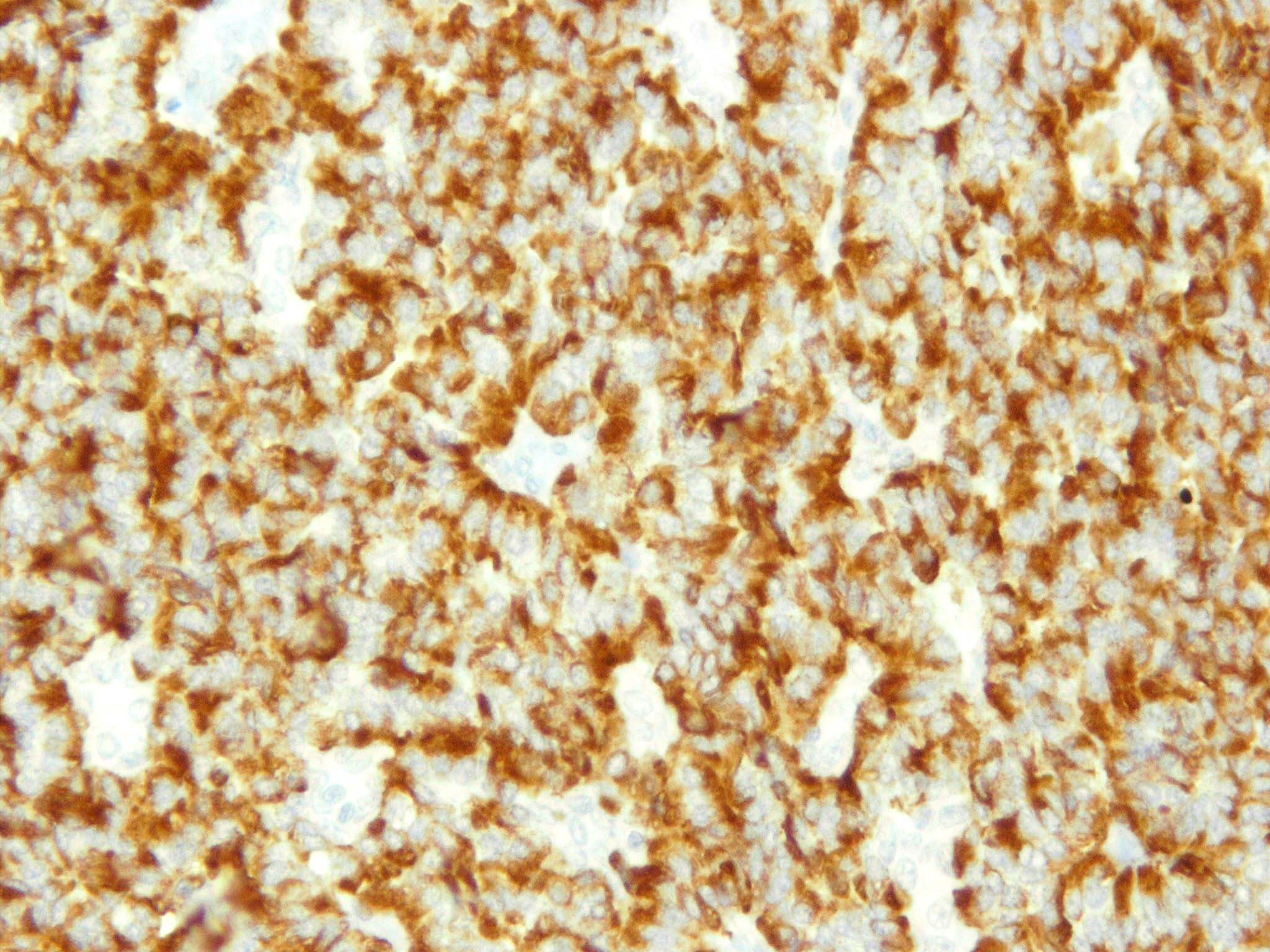
Immunostains:
Discussion:
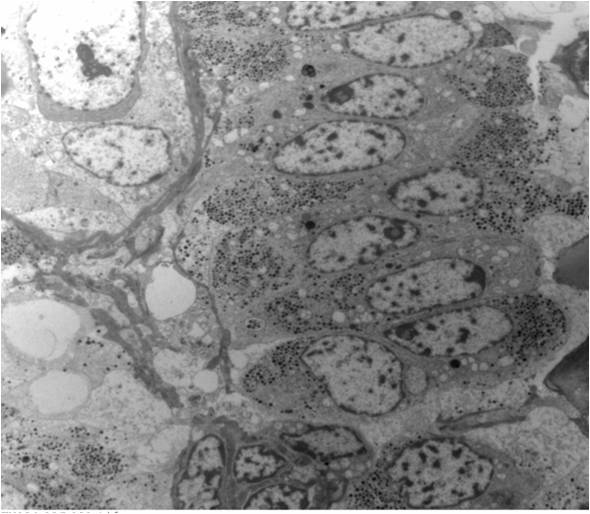
The tumor was also immunoreactive for synaptophysin and negative for CD10, RCC marker, EMA and TTF1 (images not shown). Prominent neurosecretory granules were present by electron microscopy.
Primary renal well differentiated neuroendocrine tumors (carcinoid) are rare, with < 100 cases reported. They are low grade (well differentiated) neuroendocrine tumors with low power patterns of tightly packed cords or trabeculae. The tumor cells have finely granular cytoplasm, uniform nuclei and stippled chromatin, similar to carcinoid tumors at other sites. A recent study of 9 cases, which included this case, demonstrated that perinephric extension is common (Hum Pathol 2011;42:1554).
Most tumors express either chromogranin, synaptophysin or CD56, and in one study, 8 of 9 expressed CD99. Renal carcinoid tumors are thought to derive from nonnephrogenic elements because they are negative for paired box genes 2 and 8, which are renal associated transcription factors.
The differential diagnosis of primary renal well differentiated neuroendocrine tumor (carcinoid) includes tumors with neuroendocrine appearing nuclear features or complex architectural patterns. This includes:
- Carcinoid metastatic to the kidney (BMC Urol 2010;10:22)
- Primitive neuroectodermal tumor (PNET): vaguely lobular growth of highly cellular, round to oval, poorly differentiated cells with minimal to modest pale staining cytoplasm and hyperchromatic nuclei; negative for neuroendocrine markers; 90% have EWS::FLI1 fusion product by RT-PCR
- Small cell carcinoma: diffuse growth of small cells with minimal cytoplasm, indistinct nucleoli, high mitotic activity; often extensive tumor necrosis; also Azzopardi phenomenon (blood vessels deeply encrusted with basophilic material consistent with DNA)
- Metanephric adenoma: small, uniform, closely packed tubules or papillae in loose stroma, composed of small cells with minimal cytoplasm, bland nuclei that may overlap, uniform chromatin, glomeruloid bodies, rare mitoses
- Neuroblastoma: 80% age 4 years or less; small blue cell tumor with Homer-Wright rosettes
Treatment is excision with follow up, because nodal and distant metastases are common.