All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Ankur Sangoi, Stanford University, Stanford, California, USA.
Attend the
Annual Summer Update in Clinical Immunology,
Microbiology and Infectious Diseases
July 14-18, 2008
Snow King Resort
Jackson, Wyoming (USA)

This 25.75-hour review and update in clinical immunology, microbiology and infectious diseases is intended to improve knowledge about the pathogenesis and clinical manifestations of infectious diseases, immunological mechanisms of disease and disease prevention, appropriate approaches to the diagnosis of infections and immunologic disorders, and utilization of the clinical microbiology and immunology laboratory, including selection and interpretation of results.
This course will provide a forum for the exchange of ideas dealing with microbial infections as well as immunity to infectious diseases and immunologic disorders.
Case #120
Clinical history:
An 88 year old woman presented with a cough. A CBC (complete blood count) and peripheral smear were obtained.
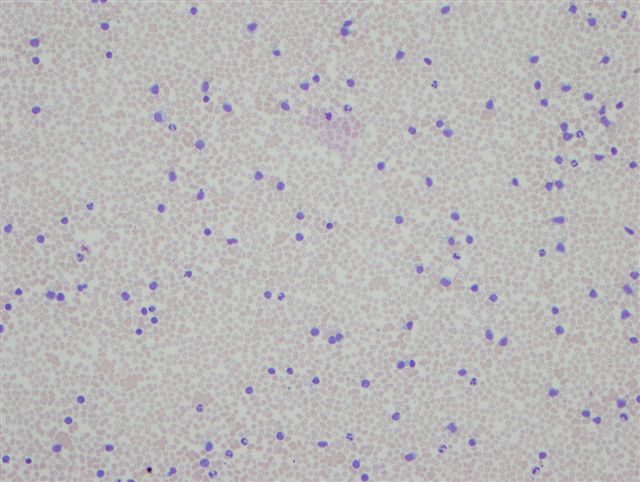
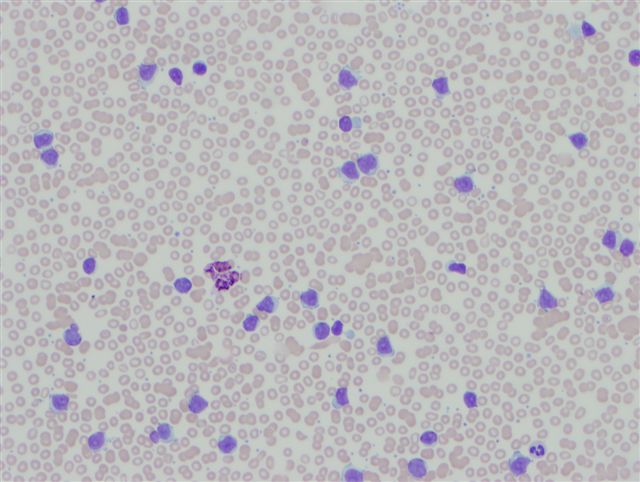
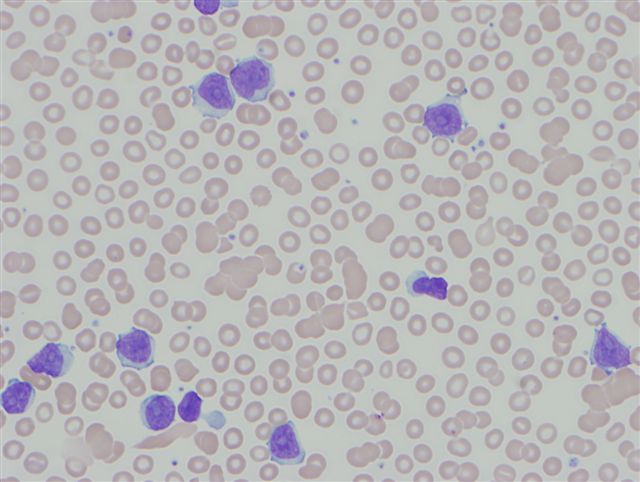
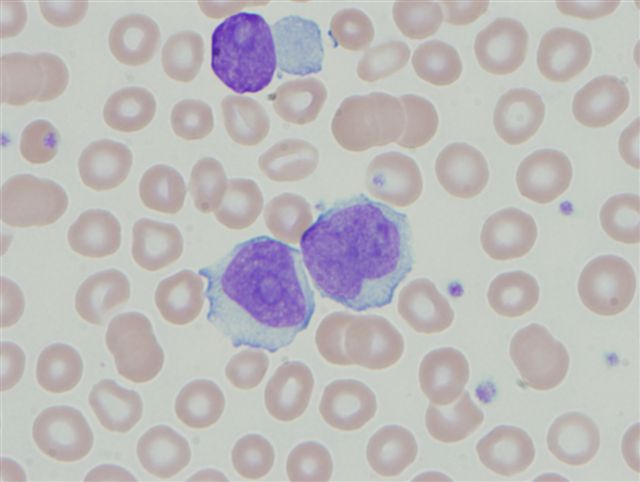
Peripheral smear (blood):
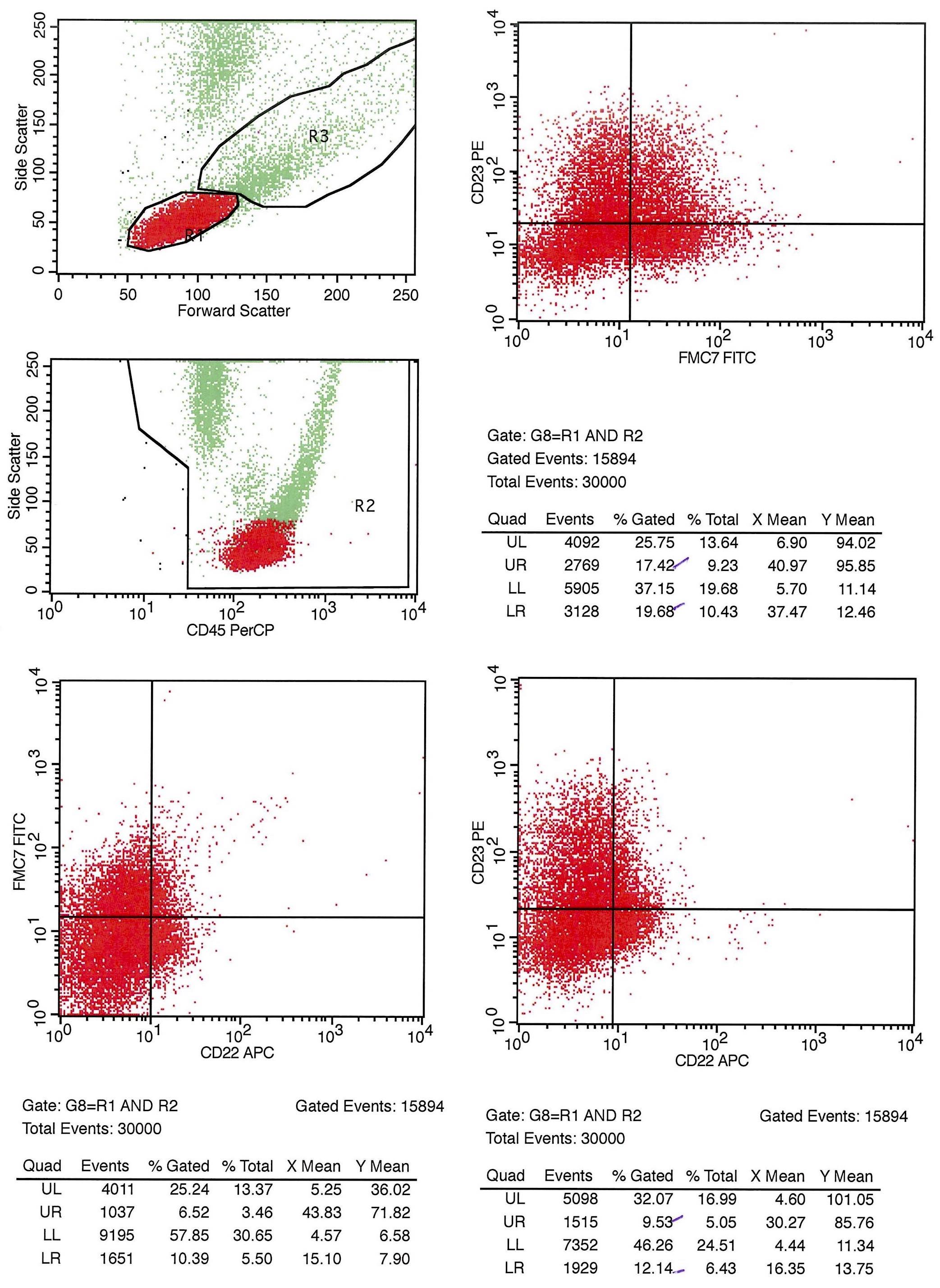
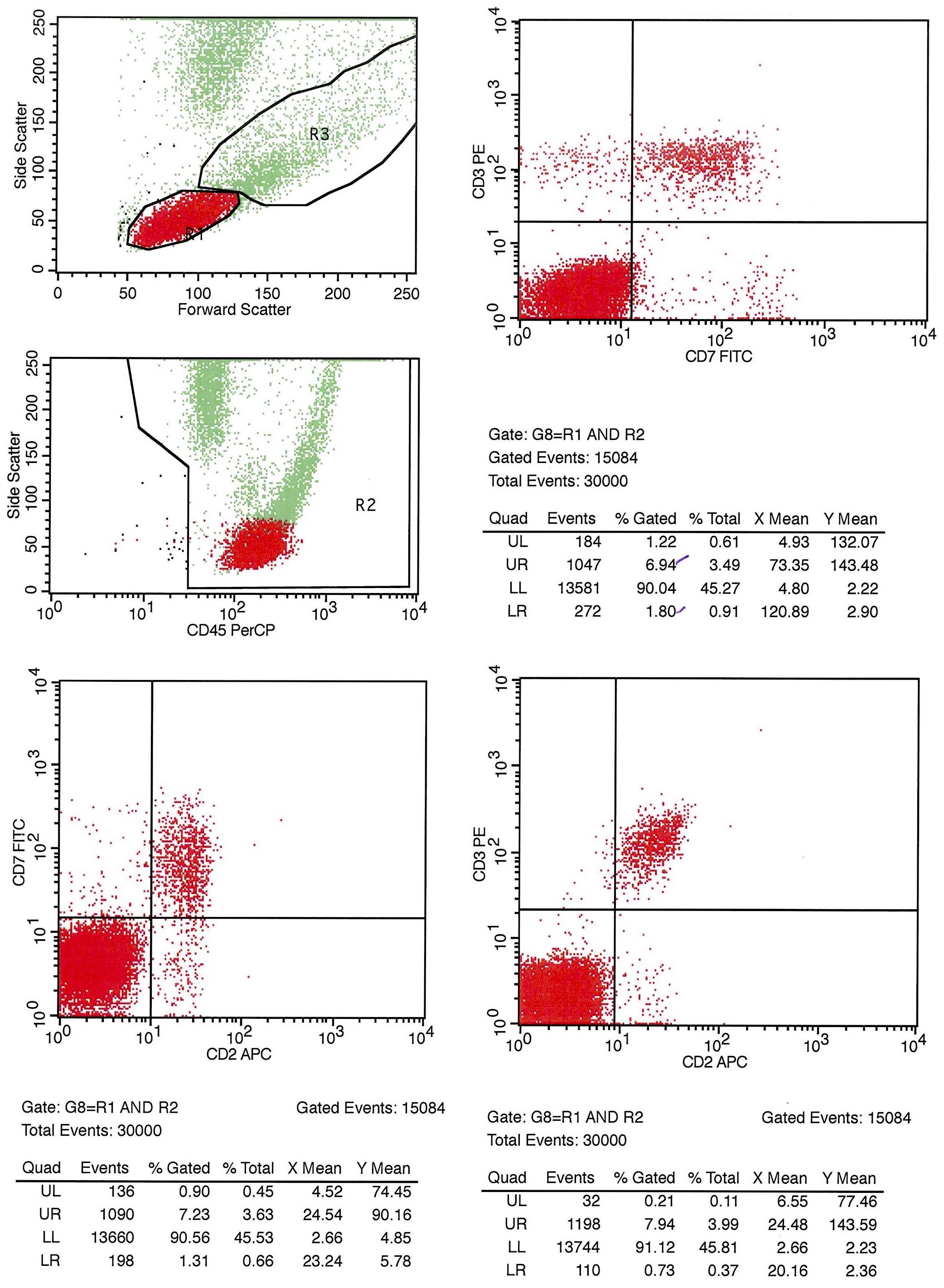
Flow cytometry images:
What is your diagnosis?
Diagnosis: B cell prolymphocytic leukemia
Discussion:
The peripheral smear shows a relatively monomorphic population of large lymphocytes with scant basophilic agranular cytoplasm, round / polygonal nuclei with occasional grooves and large, prominent nucleoli.
Flow cytometry shows a monomorphic B cell population which accounts for the majority of lymphocytes and which expresses CD19, CD20 and CD5, with bright monotypic kappa light chain restriction and dim / partial expression of CD22, CD23 and FMC7. These findings are diagnostic of B cell prolymphocytic leukemia (B-PLL).
B cell prolymphocytic leukemia (B-PLL) is a rare chronic lymphoid leukemia that typically affects elderly men, who present with a peripheral blood lymphocytosis > 100,000, marked splenomegaly and pancytopenia. By definition, prolymphocytes comprise more than 55% of the leukemic infiltrate. The prolymphocytes are found in the splenic red and white pulp, as well as in the peripheral blood. Most (80%) cases are B cell phenotype.
The differential diagnosis includes prolymphocytic transformation of chronic lymphocytic leukemia (CLL) (patient has prior history of CLL or presence of CLL cells), as well as the blastic variant of mantle cell lymphoma, which occasionally presents with more than 55% prolymphocytes but is positive for t(11;14) (Am J Clin Pathol 2001;115:571, Am J Clin Pathol 2002;117:246).
B cell prolymphocytic leukemia (B-PLL) patients have a better prognosis than T prolymphocytic leukemia (T-PLL) patients, although the disease is still considered incurable. Treatment, for symptomatic patients only, consists of monoclonal antibodies, high dose chemotherapy followed by stem cell transplantation or fludarabine-like drugs (Ann Hematol 2004;83:319, Med Sci Monit 2007;13:RA69).