9 August 2007 - Case #92
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Juan Jose Segura Fonseca, Hospital San Juan de Dios, San Jose, Costa Rica. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Case #92
Clinical history:
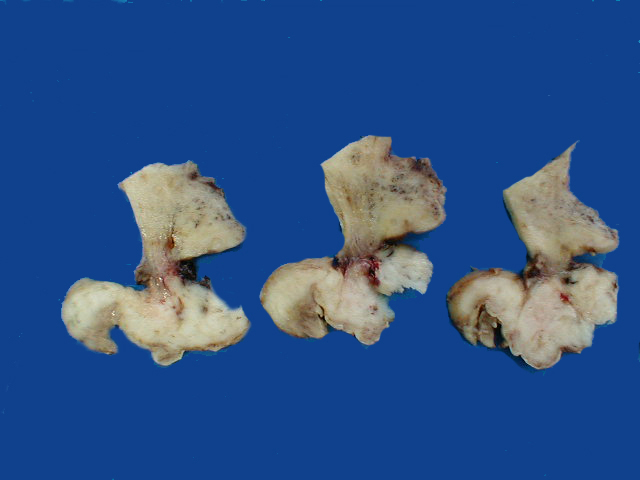
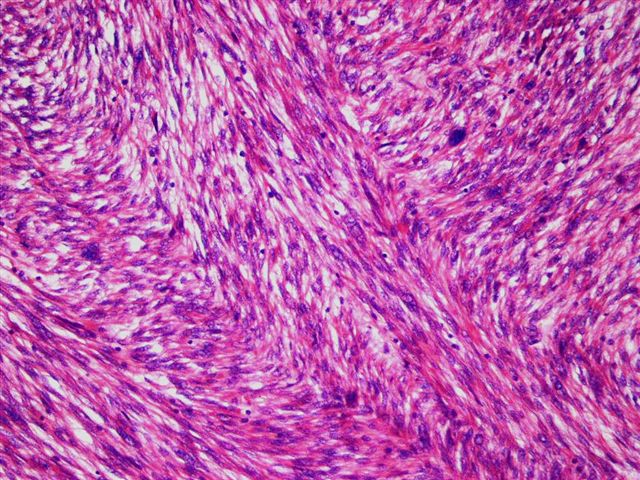
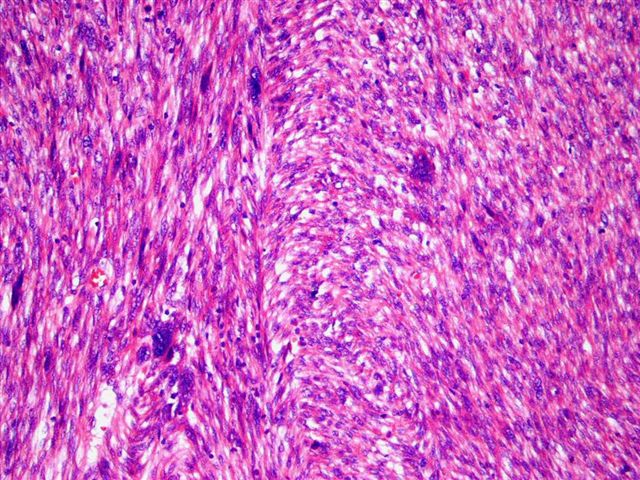
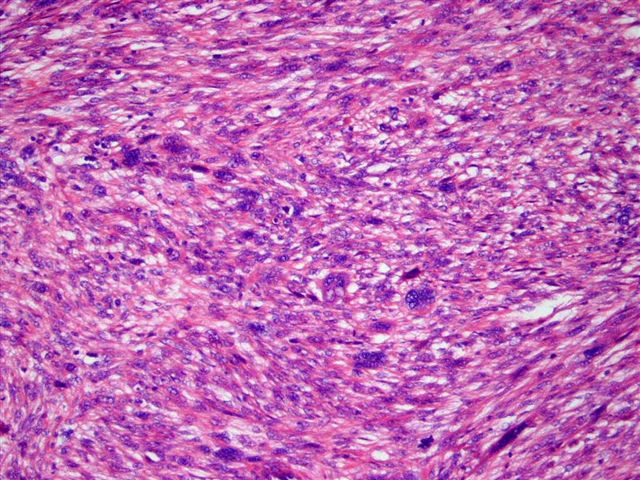
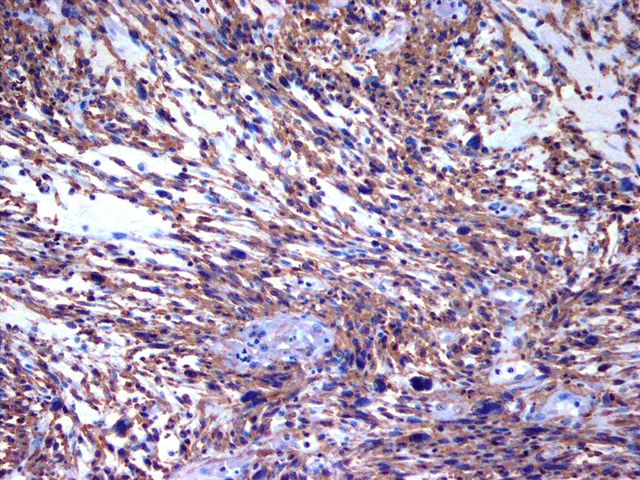
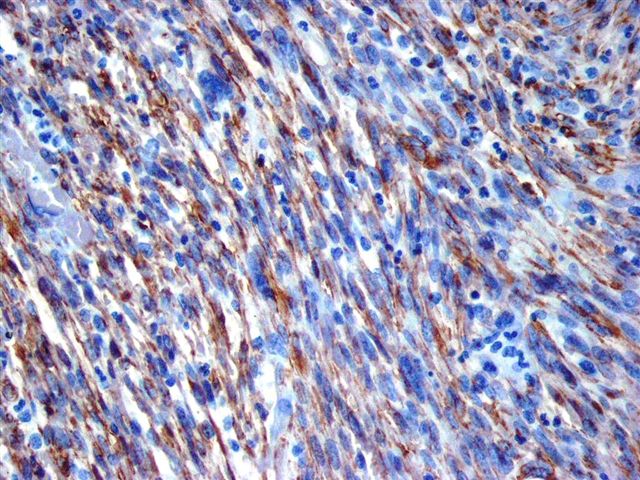
A 59 year old woman complained of abundant vaginal serosanguinous discharge and occasional bleeding during sexual intercourse. On physical examination, a tumor in the vagina was suspected. A small biopsy was diagnosed as a high grade sarcoma NOS. A total hysterectomy was performed. The uterus contained a large, multinodular, solid and polypoid tumor protruding from the cervical canal and attached by a short pedicle, more clearly shown on sagittal section. Microscopically, smooth muscle cells were arranged in interlacing fascicles, with large pleomorphic nuclei. Several mitotic figures were present. Strong immunoreactivity for muscle specific actin and smooth muscle actin was present.
Gross images:
Microscopic images:
What is your diagnosis?
Diagnosis: Leiomyosarcoma of the cervix
Discussion:
An estimated 10,520 new malignancies of the uterine cervix were diagnosed in 2004 in the United States (CA Cancer J Clin 2004;54:8). Pure cervical sarcomas are rare. Young estimated that sarcomas constituted 0.55% of cervical malignancies in the U.S. during 1973 to 1977 and Wright identified only 8 pure sarcomas in 1583 cervical malignancies (0.5%) during 1986 to 2003 (Diagn Pathol 2006;1:30, Gynecol Oncol 2005;99:348).
As a primary cervical tumor, leiomyosarcoma is very rare, particularly if cases with possible origin in the lower uterine segment are excluded. However, definitive cases have been reported after subtotal or supracervical hysterectomy for other reasons (Ginekol Pol 2002;73:613). Fadare found only 30 reported cases of primary cervical leiomyosarcoma after literature review. They occur in peri and postmenopausal women ages 40 to 60 years and most commonly present with abnormal vaginal bleeding, abdominopelvic pain and a palpable cervical mass.
Grossly, cervical leiomyosarcomas are typically large, up to 12 cm, and either protrude from the cervical canal as large polypoid tumors or thicken and expand it circumferentially. Microscopically they display typical features of classic leiomyosarcoma but may also be epithelioid, myxoid or xanthomatous (Gynecol Oncol 2005;97:957, Int J Gynecol Pathol 1998;17:89).
The differential diagnosis depends on the features present and may include melanoma, metastatic carcinoma, epithelioid sarcoma or myxoid tumors.
Prognosis is poor, often with death due to distant metastases (Cancer 1973;31:1176).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Juan Jose Segura Fonseca, Hospital San Juan de Dios, San Jose, Costa Rica. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Website news:
(1) We recently posted a new chapter on Clinical Chemistry, which contains information on thyroid function tests useful to pathologists and other laboratory personnel. Additional tests will be added over time.
Visit and follow our Blog to see recent updates to the website.
(1) We recently posted a new chapter on Clinical Chemistry, which contains information on thyroid function tests useful to pathologists and other laboratory personnel. Additional tests will be added over time.
Visit and follow our Blog to see recent updates to the website.
Case #92
Clinical history:
A 59 year old woman complained of abundant vaginal serosanguinous discharge and occasional bleeding during sexual intercourse. On physical examination, a tumor in the vagina was suspected. A small biopsy was diagnosed as a high grade sarcoma NOS. A total hysterectomy was performed. The uterus contained a large, multinodular, solid and polypoid tumor protruding from the cervical canal and attached by a short pedicle, more clearly shown on sagittal section. Microscopically, smooth muscle cells were arranged in interlacing fascicles, with large pleomorphic nuclei. Several mitotic figures were present. Strong immunoreactivity for muscle specific actin and smooth muscle actin was present.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Leiomyosarcoma of the cervix
Discussion:
An estimated 10,520 new malignancies of the uterine cervix were diagnosed in 2004 in the United States (CA Cancer J Clin 2004;54:8). Pure cervical sarcomas are rare. Young estimated that sarcomas constituted 0.55% of cervical malignancies in the U.S. during 1973 to 1977 and Wright identified only 8 pure sarcomas in 1583 cervical malignancies (0.5%) during 1986 to 2003 (Diagn Pathol 2006;1:30, Gynecol Oncol 2005;99:348).
As a primary cervical tumor, leiomyosarcoma is very rare, particularly if cases with possible origin in the lower uterine segment are excluded. However, definitive cases have been reported after subtotal or supracervical hysterectomy for other reasons (Ginekol Pol 2002;73:613). Fadare found only 30 reported cases of primary cervical leiomyosarcoma after literature review. They occur in peri and postmenopausal women ages 40 to 60 years and most commonly present with abnormal vaginal bleeding, abdominopelvic pain and a palpable cervical mass.
Grossly, cervical leiomyosarcomas are typically large, up to 12 cm, and either protrude from the cervical canal as large polypoid tumors or thicken and expand it circumferentially. Microscopically they display typical features of classic leiomyosarcoma but may also be epithelioid, myxoid or xanthomatous (Gynecol Oncol 2005;97:957, Int J Gynecol Pathol 1998;17:89).
The differential diagnosis depends on the features present and may include melanoma, metastatic carcinoma, epithelioid sarcoma or myxoid tumors.
Prognosis is poor, often with death due to distant metastases (Cancer 1973;31:1176).