25 January 2007 - Case #71
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Professor D. Y. Cohen, Herzliyah Medical Center, Israel.

Practice management services to increase your income
Case #71
Clinical history:
A 64 year old woman had pruritic, erythematous plaques on her abdomen and back that appeared and disappeared randomly. She also had a long history of smoking. The clinical concerns were mycosis fungoides or morphea (localized scleroderma). An ellipse of skin on the abdominal wall was excised.
Microscopic description:
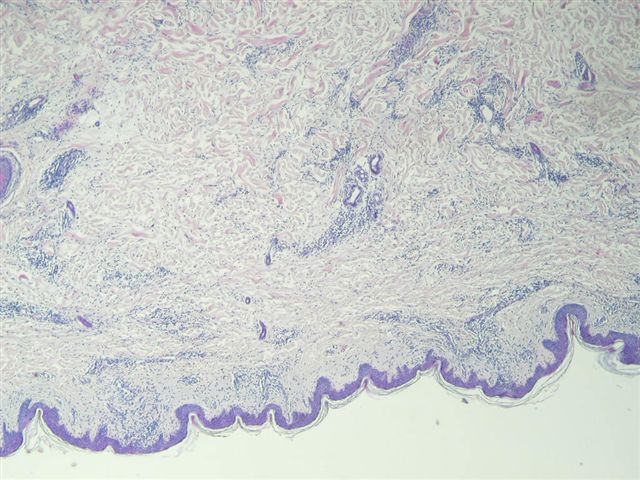
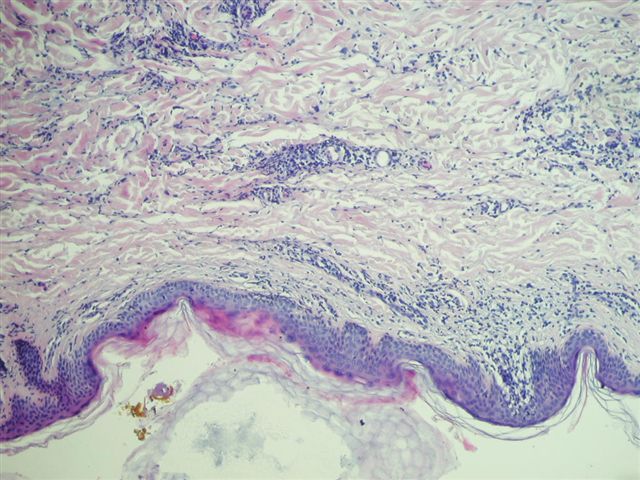
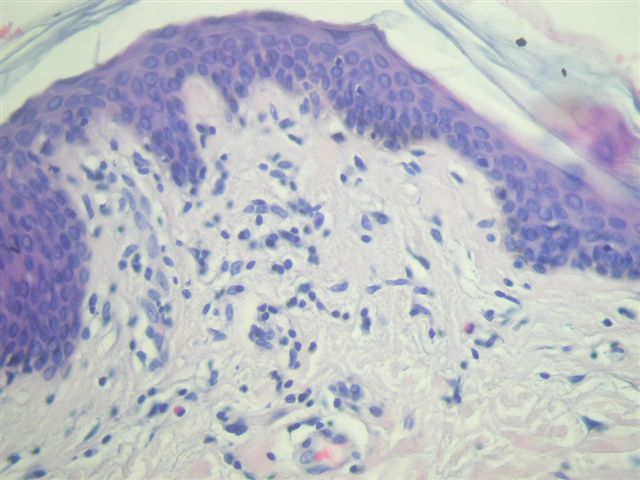
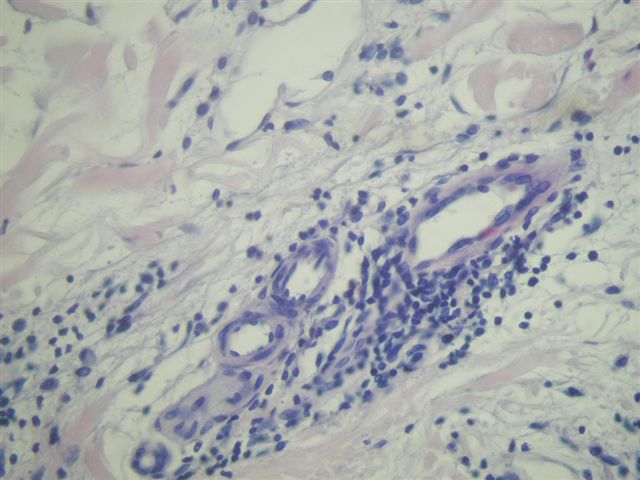
The skin biopsy shows epidermis, dermis and subcutis. The epidermis shows focal acanthosis, parakeratosis and spongiosis. There are no blisters or intraepithelial microabscesses and exocytosis (inflammatory cells in the epidermis) is minimal. The dermis shows a patchy and perivascular infiltrate which consists of small, round, mature appearing lymphocytes, as well as some histiocytes and eosinophils.
Microscopic images:
What is your diagnosis?
Diagnosis: Consistent with erythema gyratum repens
Discussion:
This case illustrates a problematic area for many pathologists - interpreting an inflammatory dermatosis. In these cases, input from the dermatologist is crucial in providing the correct diagnosis.
Erythema gyratum repens is very rare. The diagnosis is important because it is associated with existing or subsequent internal malignancy in 80% of cases (Am J Med Sci 2001;321:302). It typically causes concentric and parallel bands of erythema and scale (wood grain pattern) on the trunk and extremities (clinical image). The rash migrates at the rate of 1 cm per day and is very pruritic. It is associated with ichthyosis (16%) and hyperkeratosis (10%).
The histology is nonspecific, with mild acanthosis and spongiosis and focal parakeratosis. The dermis shows a superficial perivascular infiltrate of lymphocytes and histiocytes, with variable eosinophils and melanophages. There may be exocytosis of neutrophils and eosinophils.
The differential diagnosis include erythema annulare centrifugum. This is a hypersensitivity reaction that also grows over a period of weeks, is mildly pruritic and affects the trunk and proximal extremities. Most cases resolve within 6 weeks. Histologically, there may be a superficial perivascular infiltrate but it shows tight cuffing of the inflammatory cells around swollen endothelial cells and focal extravasation of red blood cells into the papillary dermis. The deep variant shows a coat sleeve-like pattern of perivascular infiltrate in the middle to deep dermis.
The cause of erythema gyratum repens is unknown but may have an immunological basis due to the occasional presence of C3, C4 and IgG at the basement membrane zone with direct immunofluorescence. It may also be considered a paraneoplastic syndrome. Treatment of the underlying malignancy may cause remission.
References: Medscape: Erythema Gyratum Repens [Accessed 5 April 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Professor D. Y. Cohen, Herzliyah Medical Center, Israel.

Practice management services to increase your income
Website news:
(1) This case is sponsored by Vachette Pathology. Imagine someone that solves your billing and payment problems, someone who guarantees to help you put more money back into your pocket. You do not have to change billing agents to increase your income. You simply have to manage the process. Who's watching your wallet?
Vachette Pathology is a Pathology Practice Management Firm, we are not a billing agency; what we do is manage your financial bloodline. We will push your billing process to optimum performance, renegotiate your manage care contracts and help with the business of pathology, all to ensure your financial future. For further information, please contact Mick Raich at: mraich@vachettepathology.com or call at 866-407-0763.
Visit and follow our Blog to see recent updates to the website.
(1) This case is sponsored by Vachette Pathology. Imagine someone that solves your billing and payment problems, someone who guarantees to help you put more money back into your pocket. You do not have to change billing agents to increase your income. You simply have to manage the process. Who's watching your wallet?
Vachette Pathology is a Pathology Practice Management Firm, we are not a billing agency; what we do is manage your financial bloodline. We will push your billing process to optimum performance, renegotiate your manage care contracts and help with the business of pathology, all to ensure your financial future. For further information, please contact Mick Raich at: mraich@vachettepathology.com or call at 866-407-0763.
Visit and follow our Blog to see recent updates to the website.
Case #71
Clinical history:
A 64 year old woman had pruritic, erythematous plaques on her abdomen and back that appeared and disappeared randomly. She also had a long history of smoking. The clinical concerns were mycosis fungoides or morphea (localized scleroderma). An ellipse of skin on the abdominal wall was excised.
Microscopic description:
The skin biopsy shows epidermis, dermis and subcutis. The epidermis shows focal acanthosis, parakeratosis and spongiosis. There are no blisters or intraepithelial microabscesses and exocytosis (inflammatory cells in the epidermis) is minimal. The dermis shows a patchy and perivascular infiltrate which consists of small, round, mature appearing lymphocytes, as well as some histiocytes and eosinophils.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Consistent with erythema gyratum repens
Discussion:
This case illustrates a problematic area for many pathologists - interpreting an inflammatory dermatosis. In these cases, input from the dermatologist is crucial in providing the correct diagnosis.
Erythema gyratum repens is very rare. The diagnosis is important because it is associated with existing or subsequent internal malignancy in 80% of cases (Am J Med Sci 2001;321:302). It typically causes concentric and parallel bands of erythema and scale (wood grain pattern) on the trunk and extremities (clinical image). The rash migrates at the rate of 1 cm per day and is very pruritic. It is associated with ichthyosis (16%) and hyperkeratosis (10%).
The histology is nonspecific, with mild acanthosis and spongiosis and focal parakeratosis. The dermis shows a superficial perivascular infiltrate of lymphocytes and histiocytes, with variable eosinophils and melanophages. There may be exocytosis of neutrophils and eosinophils.
The differential diagnosis include erythema annulare centrifugum. This is a hypersensitivity reaction that also grows over a period of weeks, is mildly pruritic and affects the trunk and proximal extremities. Most cases resolve within 6 weeks. Histologically, there may be a superficial perivascular infiltrate but it shows tight cuffing of the inflammatory cells around swollen endothelial cells and focal extravasation of red blood cells into the papillary dermis. The deep variant shows a coat sleeve-like pattern of perivascular infiltrate in the middle to deep dermis.
The cause of erythema gyratum repens is unknown but may have an immunological basis due to the occasional presence of C3, C4 and IgG at the basement membrane zone with direct immunofluorescence. It may also be considered a paraneoplastic syndrome. Treatment of the underlying malignancy may cause remission.
References: Medscape: Erythema Gyratum Repens [Accessed 5 April 2024]