26 October 2006 - Case #63
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Sharon Bihlmeyer, University of Vermont, Burlington, Vermont, USA.
Case #63
Clinical history:
A 53 year old man presented with a 4 month history of a protuberant and painful left anterior pretribial mass. 11 years previously, he had an excision of a similar mass in the same location. Metabolic laboratory studies were within normal limits, including a phosphorus level of 4.4 mg/dL. An excisional biopsy was performed.
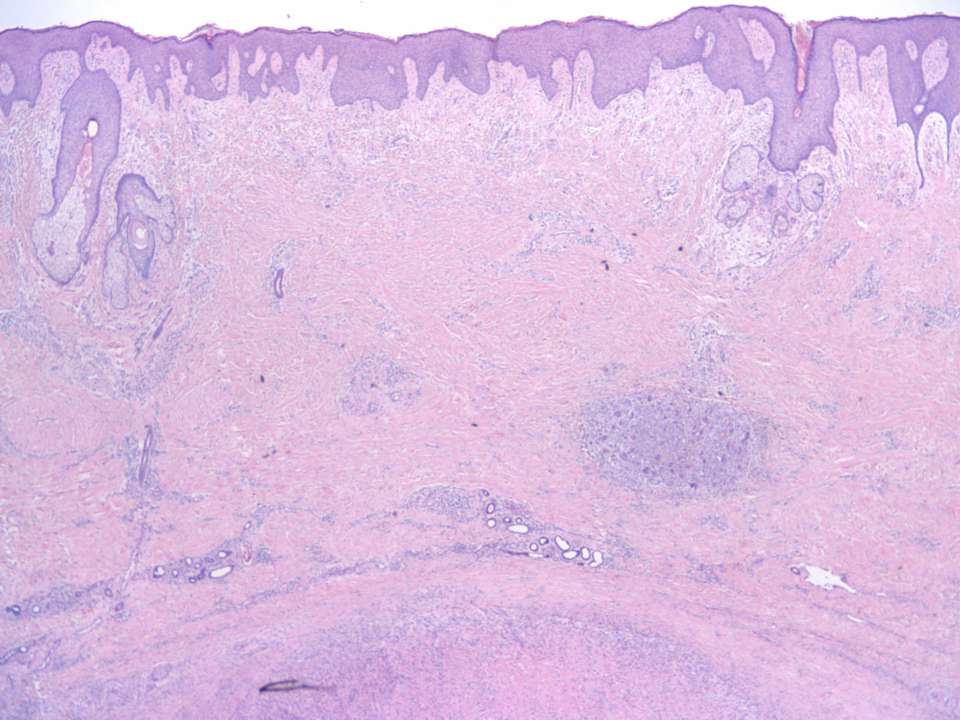
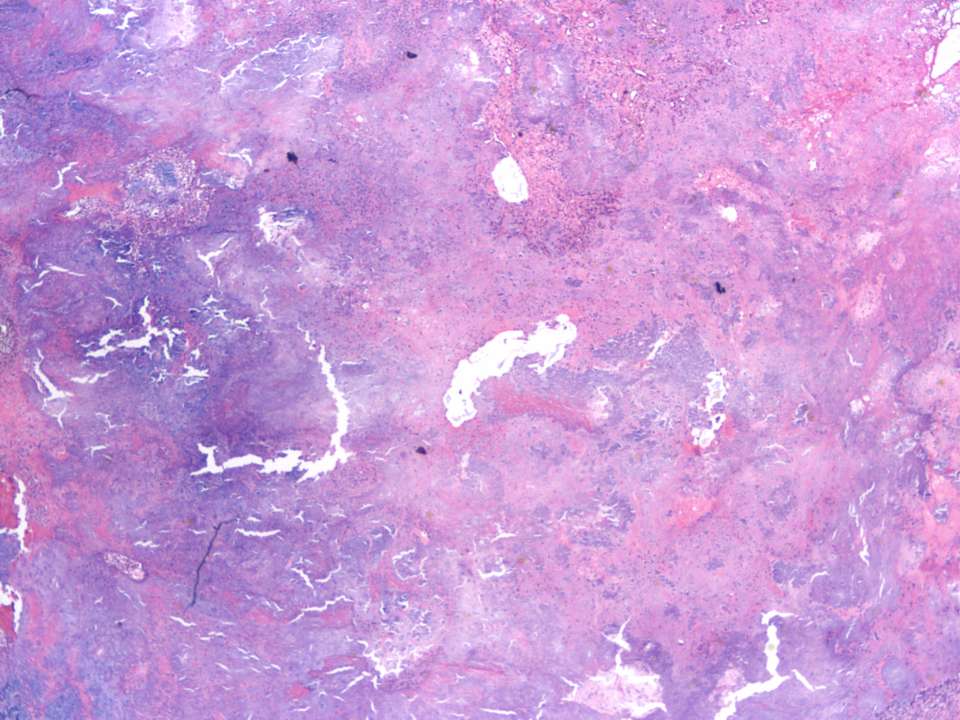
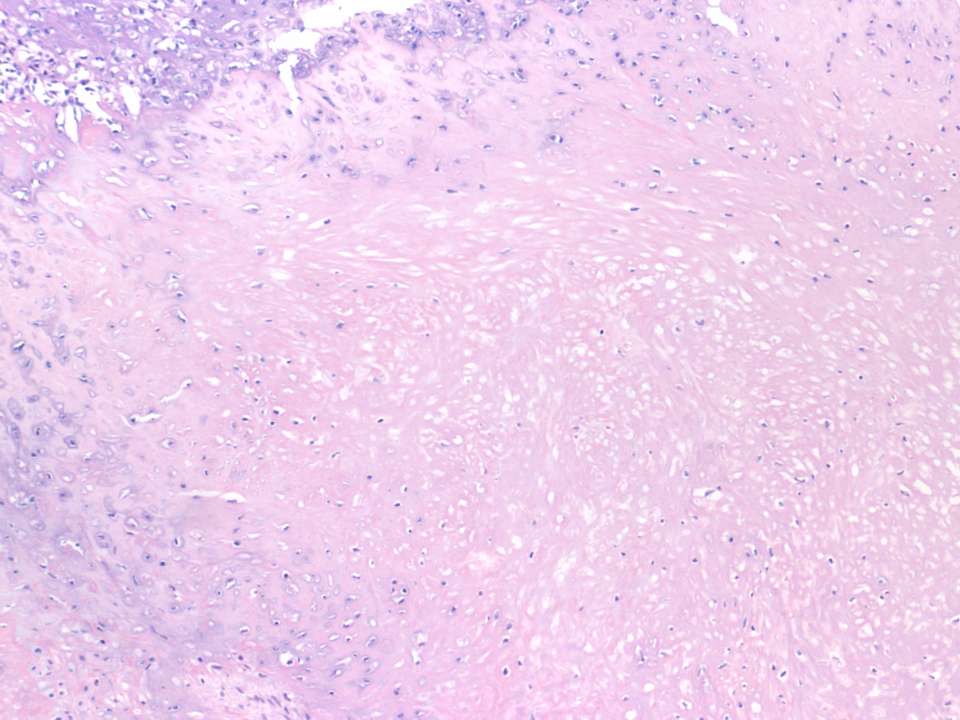
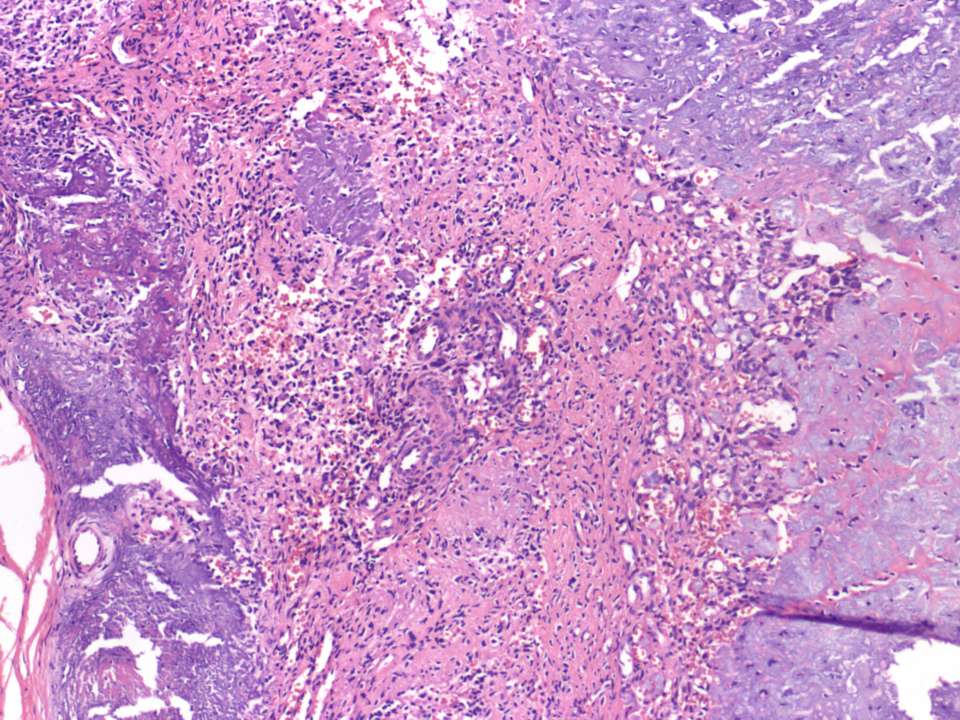
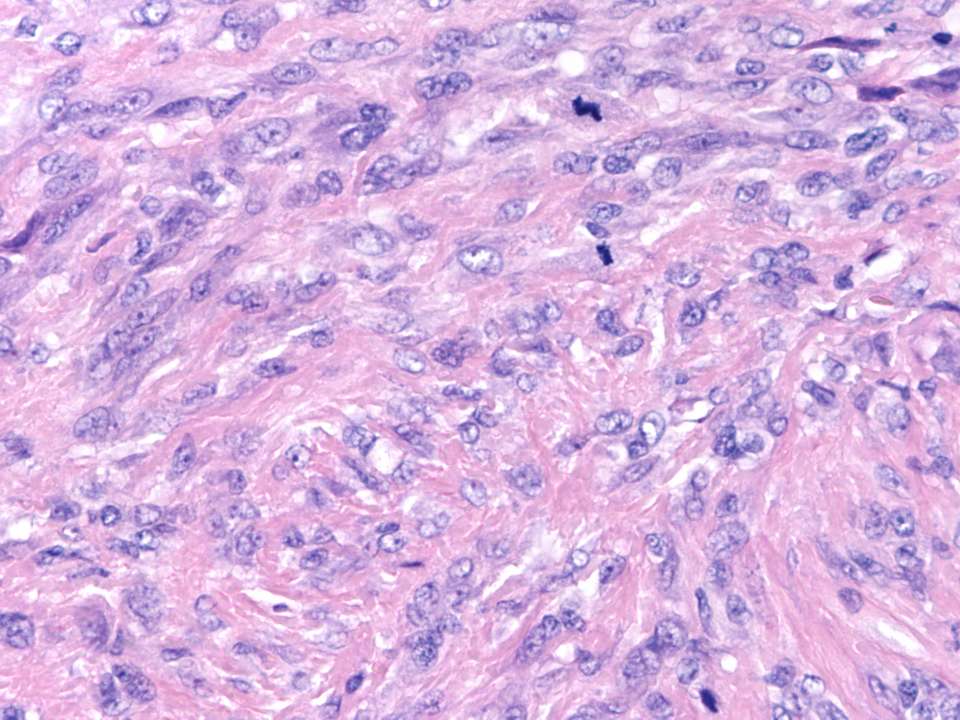
Microscopic images:
What is your diagnosis?
Diagnosis: Phosphaturic mesenchymal tumor
Discussion:
Phosphaturic mesenchymal tumor is extremely rare. It affects women slightly more commonly than men, with a median age 53 years but a wide range of 9 - 80 years.
This tumor often produce oncogenic osteomalacia, characterized by low serum phosphate, reduced tubular reabsorption of phosphate and a low or inappropriately normal 1,25 dihydroxy vitamin D. In children, it may cause rickets (Pediatr Dev Pathol 2000;3:61).
These tumors are usually benign and complete excision typically causes dramatic reversal of the endocrine signs and symptoms (Am J Surg Pathol 1989;13:588).
Grossly, the tumors may be up to 14 cm and arise in soft tissue and bone. They are hypocellular, composed of bland spindled cells with small nuclei and indistinct nucleoli, as well as osteoclast-like giant cells. The stroma exhibits myxoid change, a distinctive grungy calcified matrix, metaplastic bone and fat. There may be hemangiopericytoma-like vessels, microcysts and hemorrhage. The tumors are infiltrative but there is typically no / rare mitotic activity and no atypia. Cases are considered malignant if they have nuclear atypia, high cellularity and 5+ mitotic figures/10 high power fields.
Immunohistochemistry is not routinely used. However, the tumor cells are immunoreactive for fibroblast growth factor 23 and dentin matrix protein 1, which are thought to mediate their metabolic effects and may be useful in difficult cases (Am J Surg Pathol 2004;28:1, Mod Pathol 2004;17:573).
The differential diagnosis includes other mesenchymal tumors, such as hemangiopericytoma, osteosarcoma and giant cell tumor.
This case showed a normal phosphorus, which is not typical, and some mitotic figures. However, the diagnosis was confirmed by Dr. Christopher Fletcher at Harvard.
References: Cancer 1987;59:1442, Arch Pathol Lab Med 2002;126:1245 (case report of 36 year old woman with muscle pain and weakness)
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Sharon Bihlmeyer, University of Vermont, Burlington, Vermont, USA.
Website news:
(1) How can you find detailed pathology information in 15 seconds or less? Use our free online textbook. From the Home page at www.PathologyOutlines.com, click on the appropriate chapter, then on the topic in the Table of Contents and you will be directed to clinical information, gross and microscopic images, immunohistochemistry and other stain results, references and other pertinent information. This is a good way to quickly refresh your memory on any entity you have not seen in a while.
Visit and follow our Blog to see recent updates to the website.
(1) How can you find detailed pathology information in 15 seconds or less? Use our free online textbook. From the Home page at www.PathologyOutlines.com, click on the appropriate chapter, then on the topic in the Table of Contents and you will be directed to clinical information, gross and microscopic images, immunohistochemistry and other stain results, references and other pertinent information. This is a good way to quickly refresh your memory on any entity you have not seen in a while.
Visit and follow our Blog to see recent updates to the website.
Case #63
Clinical history:
A 53 year old man presented with a 4 month history of a protuberant and painful left anterior pretribial mass. 11 years previously, he had an excision of a similar mass in the same location. Metabolic laboratory studies were within normal limits, including a phosphorus level of 4.4 mg/dL. An excisional biopsy was performed.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Phosphaturic mesenchymal tumor
Discussion:
Phosphaturic mesenchymal tumor is extremely rare. It affects women slightly more commonly than men, with a median age 53 years but a wide range of 9 - 80 years.
This tumor often produce oncogenic osteomalacia, characterized by low serum phosphate, reduced tubular reabsorption of phosphate and a low or inappropriately normal 1,25 dihydroxy vitamin D. In children, it may cause rickets (Pediatr Dev Pathol 2000;3:61).
These tumors are usually benign and complete excision typically causes dramatic reversal of the endocrine signs and symptoms (Am J Surg Pathol 1989;13:588).
Grossly, the tumors may be up to 14 cm and arise in soft tissue and bone. They are hypocellular, composed of bland spindled cells with small nuclei and indistinct nucleoli, as well as osteoclast-like giant cells. The stroma exhibits myxoid change, a distinctive grungy calcified matrix, metaplastic bone and fat. There may be hemangiopericytoma-like vessels, microcysts and hemorrhage. The tumors are infiltrative but there is typically no / rare mitotic activity and no atypia. Cases are considered malignant if they have nuclear atypia, high cellularity and 5+ mitotic figures/10 high power fields.
Immunohistochemistry is not routinely used. However, the tumor cells are immunoreactive for fibroblast growth factor 23 and dentin matrix protein 1, which are thought to mediate their metabolic effects and may be useful in difficult cases (Am J Surg Pathol 2004;28:1, Mod Pathol 2004;17:573).
The differential diagnosis includes other mesenchymal tumors, such as hemangiopericytoma, osteosarcoma and giant cell tumor.
This case showed a normal phosphorus, which is not typical, and some mitotic figures. However, the diagnosis was confirmed by Dr. Christopher Fletcher at Harvard.
References: Cancer 1987;59:1442, Arch Pathol Lab Med 2002;126:1245 (case report of 36 year old woman with muscle pain and weakness)