21 June 2006 - Case #50
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.

This Case is sponsored by Sakura Finetek, USA. Leading the revolution in Pathology, the Tissue-Tek Xpress Rapid Tissue Processor is helping laboratories achieve new levels of productivity. Enabling a continuous flow of up to 40 cassettes every 15 minutes, this system can process up to 120 specimens per hour. The Xpress allows for a balanced distribution of work throughout the day, eliminating bottlenecks and batches common with overnight processing. Improved turnaround times, reduced waste and increased productivity are just a few benefits this technology can offer your lab. Results are the same or better than overnight processing. Help your lab reach its full potential with the Tissue-Tek Xpress Rapid Tissue Processor. For more information, contact Ms. Elise Green, Marketing Manager at 1-800-725-8723 extension 7873 or at egreen@sakuraus.com
We thank Dr. Victor Lee, KK Women's and Children's Hospital, Singapore, for contributing this case.
Case #50
Clinical history:
A 12 year old girl had a solitary superficial tumor of the back. She had no significant medical history.
Microscopic images:
What is your diagnosis?
Diagnosis: Plexiform schwannoma (superficial type)
Discussion:
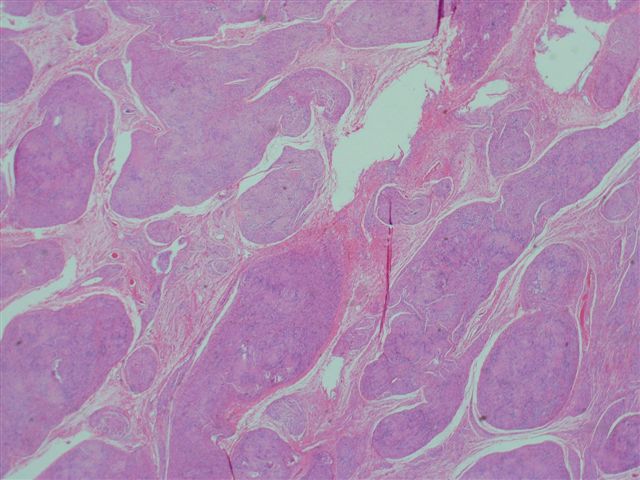
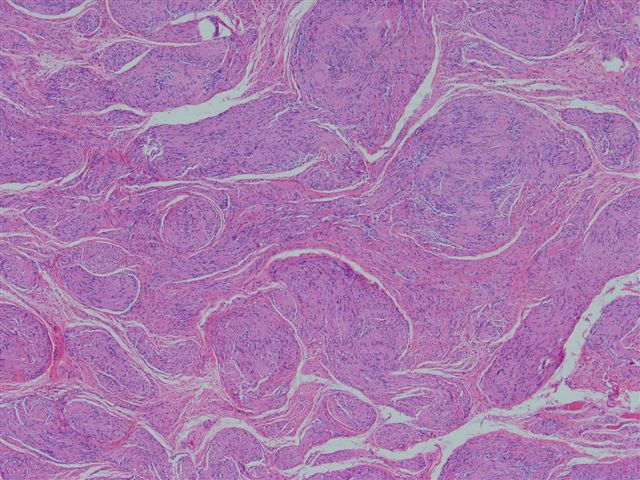
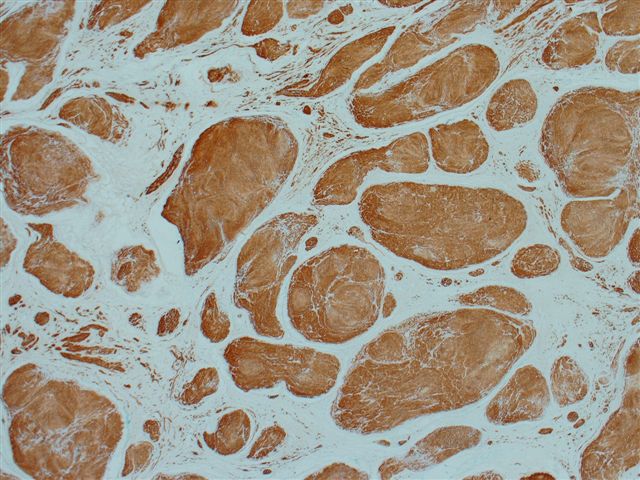
The microscopic images show a plexiform architecture, with nuclear palisading identifiable at medium power. Although schwannomas usually have a biphasic pattern of Antoni A (short fascicles of spindle cells with nuclear palisading and Verocay bodies) and Antoni B areas (less cellular areas with irregularly spaced vessels), it is not prominent in these images. There are also more cellular areas and strong S100 immunoreactivity.
Only 5% of schwannomas have a plexiform or multinodular growth pattern. Unlike neurofibromas, this pattern is not strongly associated with neurofibromatosis 1 or 2. These tumors usually are superficial and located in the dermis or subcutaneous tissue. They are frequently cellular with hyperchromatic nuclei and increased mitotic figures. There is usually no / minimal necrosis or myxoid change. All tumors show strong and diffuse S100 immunoreactivity of the nodules, with no staining of the intervening stroma.
The differential diagnosis includes plexiform neurofibroma and malignant peripheral nerve sheath tumor (MPNST). Plexiform neurofibromas almost always develop during early childhood and are considered pathognomonic for neurofibromatosis type 1. They are associated with grossly enlarged and tortuous nerves. Microscopically, they are hypocellular with a myxoid background and lack the biphasic pattern seen in schwannomas. However, they occasionally show nuclear palisading. Although neurofibromas are S100 immunoreactive, there is only staining of scattered cells that are diffusely throughout the lesion. In contrast, schwannomas show strong staining of the tumor nodules and no staining of the intervening stroma.
The cellularity, mitotic activity and atypia of plexiform schwannomas is also suggestive of MPNST, which may be multinodular, particularly if it arises from a plexiform neurofibroma. Before diagnosing a plexiform MPNST, it is recommended to sample the tumor extensively to rule out a plexiform schwannoma (Am J Surg Path 2005;29:1042). S100 staining may be somewhat helpful, as MPNSTs typically show negative or weak staining.
Additional references: Weiss: Enzinger and Weiss's Soft Tissue Tumors, 4th Edition, 2001
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.

This Case is sponsored by Sakura Finetek, USA. Leading the revolution in Pathology, the Tissue-Tek Xpress Rapid Tissue Processor is helping laboratories achieve new levels of productivity. Enabling a continuous flow of up to 40 cassettes every 15 minutes, this system can process up to 120 specimens per hour. The Xpress allows for a balanced distribution of work throughout the day, eliminating bottlenecks and batches common with overnight processing. Improved turnaround times, reduced waste and increased productivity are just a few benefits this technology can offer your lab. Results are the same or better than overnight processing. Help your lab reach its full potential with the Tissue-Tek Xpress Rapid Tissue Processor. For more information, contact Ms. Elise Green, Marketing Manager at 1-800-725-8723 extension 7873 or at egreen@sakuraus.com
We thank Dr. Victor Lee, KK Women's and Children's Hospital, Singapore, for contributing this case.
Case #50
Clinical history:
A 12 year old girl had a solitary superficial tumor of the back. She had no significant medical history.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Plexiform schwannoma (superficial type)
Discussion:
The microscopic images show a plexiform architecture, with nuclear palisading identifiable at medium power. Although schwannomas usually have a biphasic pattern of Antoni A (short fascicles of spindle cells with nuclear palisading and Verocay bodies) and Antoni B areas (less cellular areas with irregularly spaced vessels), it is not prominent in these images. There are also more cellular areas and strong S100 immunoreactivity.
Only 5% of schwannomas have a plexiform or multinodular growth pattern. Unlike neurofibromas, this pattern is not strongly associated with neurofibromatosis 1 or 2. These tumors usually are superficial and located in the dermis or subcutaneous tissue. They are frequently cellular with hyperchromatic nuclei and increased mitotic figures. There is usually no / minimal necrosis or myxoid change. All tumors show strong and diffuse S100 immunoreactivity of the nodules, with no staining of the intervening stroma.
The differential diagnosis includes plexiform neurofibroma and malignant peripheral nerve sheath tumor (MPNST). Plexiform neurofibromas almost always develop during early childhood and are considered pathognomonic for neurofibromatosis type 1. They are associated with grossly enlarged and tortuous nerves. Microscopically, they are hypocellular with a myxoid background and lack the biphasic pattern seen in schwannomas. However, they occasionally show nuclear palisading. Although neurofibromas are S100 immunoreactive, there is only staining of scattered cells that are diffusely throughout the lesion. In contrast, schwannomas show strong staining of the tumor nodules and no staining of the intervening stroma.
The cellularity, mitotic activity and atypia of plexiform schwannomas is also suggestive of MPNST, which may be multinodular, particularly if it arises from a plexiform neurofibroma. Before diagnosing a plexiform MPNST, it is recommended to sample the tumor extensively to rule out a plexiform schwannoma (Am J Surg Path 2005;29:1042). S100 staining may be somewhat helpful, as MPNSTs typically show negative or weak staining.
Additional references: Weiss: Enzinger and Weiss's Soft Tissue Tumors, 4th Edition, 2001