5 April 2006 - Case #42
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Janine LoBello, St. Josephs Hospital & Medical Center in Phoenix, Arizona, USA.
Case #42
Clinical history:
The patient is a 63 year old man who presented with a slowly enlarging, somewhat painful mass of the cheek. A 6.0 x 4.5 x 3.0 cm portion of soft tissue was received fresh for frozen section, which demonstrated a 2.4 x 1.0 x 0.4 cm, well circumscribed, bright yellow to dark brown and hemorrhagic mass.
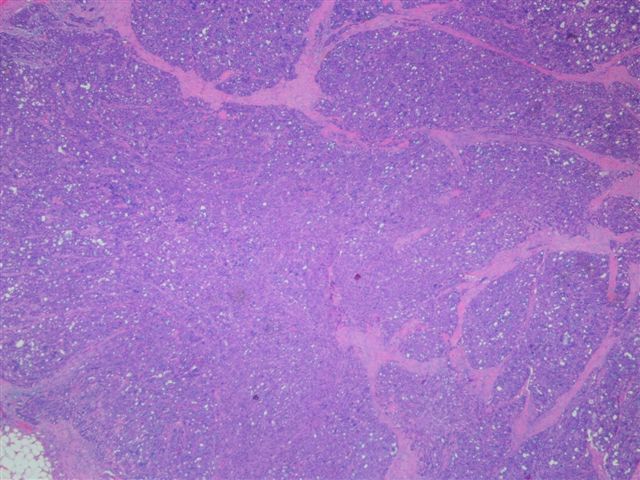
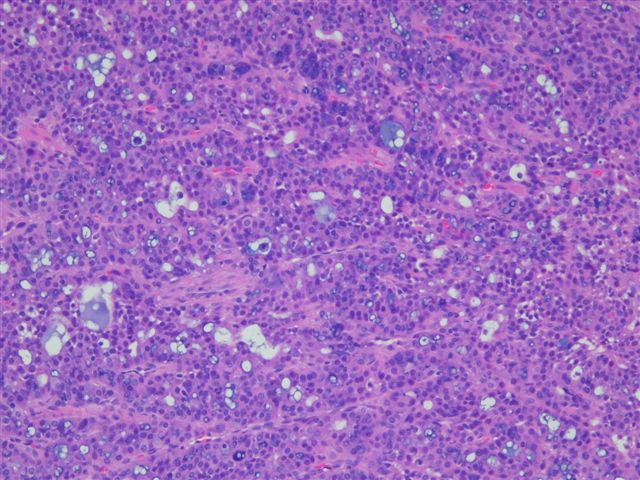
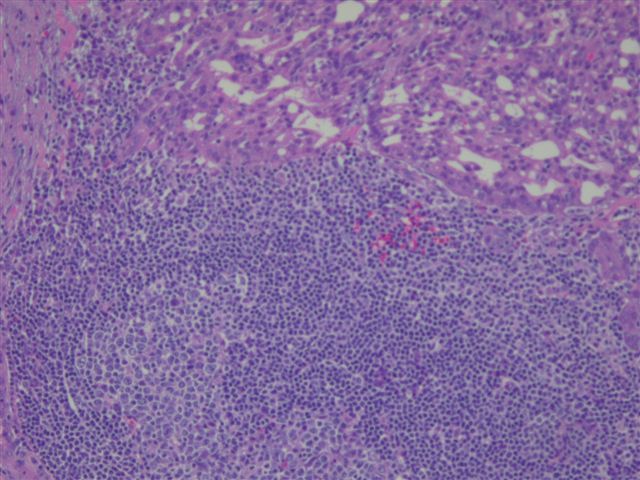
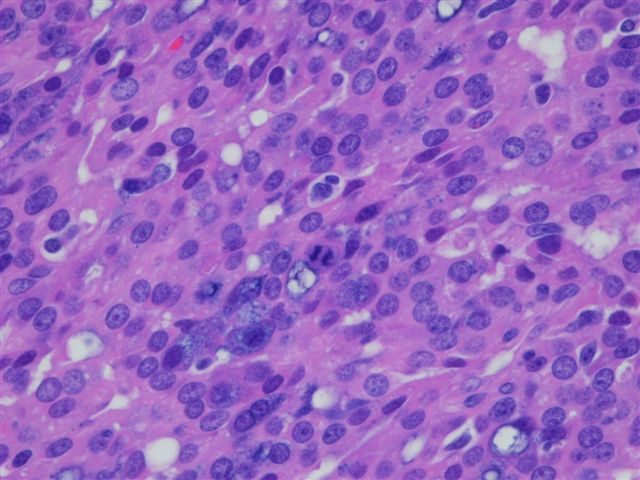
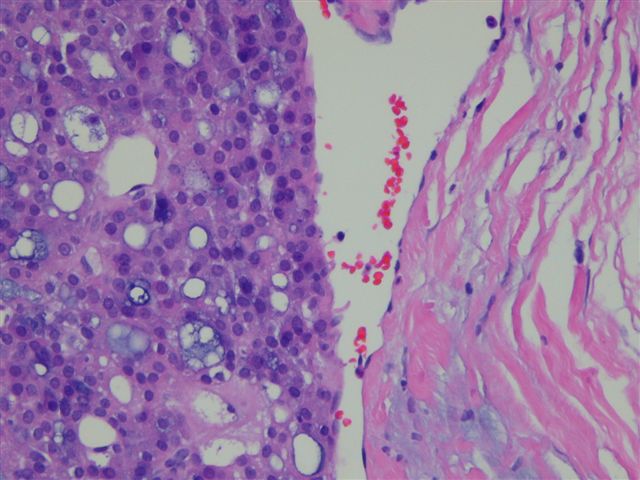
Microscopic images:
What is your diagnosis?
Diagnosis: Acinic cell carcinoma of the parotid gland
Discussion:
Although acinic cell carcinomas represent only 2 - 6% of salivary gland tumors, they are the third most common epithelial malignancy after mucoepidermoid carcinoma and adenocarcinoma, NOS and represent about 10% of all malignant salivary gland tumors. Most of these tumors occur in the parotid gland, with the remainder usually in parotid lymph nodes, the submandibular gland or minor salivary glands. The mean patient age is 44 years but they are the second most common salivary gland malignancy in children, after mucoepidermoid carcinoma.
Grossly, acinic cell carcinomas are often encapsulated, tan-gray and usually 3 cm or less. Up to 3% are bilateral or multicentric. There is usually a mixture of patterns, including solid, microcystic, papillary - cystic and follicular. However, the lobular pattern of the normal parotid gland is absent. At least a portion of the tumor demonstrates serous type acinar differentiation with large polygonal cells containing granular, PAS+ basophilic cytoplasm due to zymogen granules. The nuclei are eccentric, dark and round. There may also be clear cells containing glycogen, vacuolated cells, glandular cells and intercalated duct type cells. Lymphoid stroma may be present, as in this case (image 4) (Hum Pathol 1997;28:595). Psammoma bodies are occasionally found. The striated ducts of the normal parotid gland are lacking.
These tumors may have amylase positive cytoplasm, although immunohistochemistry is typically not helpful in diagnosis. Electron microscopy may demonstrate relatively specific, zymogen like cytoplasmic granules that are electron dense, round - oval and membrane bound. The acinar tumor cells also have a well developed rough endoplasmic reticulum similar to normal salivary glands (see figure 5).
The differential diagnosis may include normal parotid gland, which has a lobular architecture with striated and interlobular ducts, as well as acinar cells. The follicular and papillary patterns may resemble thyroid carcinoma and the papillary pattern may resemble low grade salivary duct carcinoma (Am J Surg Pathol 2004;28:1040). Fine needle aspirations must be interpreted with caution, as they are often diagnosed as benign or nonneoplastic (Curr Opin Otolaryngol Head Neck Surg 2006;14:62).
Behavior is difficult to predict from histology. However, there is some general agreement on poor prognostic factors, many present in this case. They include pleomorphism (image 5), increased mitotic activity (image 6), vascular invasion (image 7) and clinical pain or fixation. Other poor prognostic factors are high stage, positive margins, tumor necrosis, stromal hyalinization, perineural invasion, large size and involvement of the deep lobe of the parotid gland.
Approximately 10 - 15% of acinic cell carcinomas metastasize, usually to local lymph nodes. Adequate excision is important, as it reduces the recurrence rate from 80 - 90% (with inadequate excision) to 10 - 30%. The surgeon can usually spare the facial nerve (Ear Nose Throat J 2005;84:597). Radiation therapy may be useful for positive surgical margins, advanced stage or high grade histology. Overall 5 year survival is 90%, the highest among parotid gland malignancies but late deaths also occur (Am J Otolaryngol 2005;26:39).
References: Ellis: Tumors of the Salivary Glands (Atlas of Tumor Pathology, 3rd Series, Vol 17), 1996
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Janine LoBello, St. Josephs Hospital & Medical Center in Phoenix, Arizona, USA.
Case #42
Clinical history:
The patient is a 63 year old man who presented with a slowly enlarging, somewhat painful mass of the cheek. A 6.0 x 4.5 x 3.0 cm portion of soft tissue was received fresh for frozen section, which demonstrated a 2.4 x 1.0 x 0.4 cm, well circumscribed, bright yellow to dark brown and hemorrhagic mass.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Acinic cell carcinoma of the parotid gland
Discussion:
Although acinic cell carcinomas represent only 2 - 6% of salivary gland tumors, they are the third most common epithelial malignancy after mucoepidermoid carcinoma and adenocarcinoma, NOS and represent about 10% of all malignant salivary gland tumors. Most of these tumors occur in the parotid gland, with the remainder usually in parotid lymph nodes, the submandibular gland or minor salivary glands. The mean patient age is 44 years but they are the second most common salivary gland malignancy in children, after mucoepidermoid carcinoma.
Grossly, acinic cell carcinomas are often encapsulated, tan-gray and usually 3 cm or less. Up to 3% are bilateral or multicentric. There is usually a mixture of patterns, including solid, microcystic, papillary - cystic and follicular. However, the lobular pattern of the normal parotid gland is absent. At least a portion of the tumor demonstrates serous type acinar differentiation with large polygonal cells containing granular, PAS+ basophilic cytoplasm due to zymogen granules. The nuclei are eccentric, dark and round. There may also be clear cells containing glycogen, vacuolated cells, glandular cells and intercalated duct type cells. Lymphoid stroma may be present, as in this case (image 4) (Hum Pathol 1997;28:595). Psammoma bodies are occasionally found. The striated ducts of the normal parotid gland are lacking.
These tumors may have amylase positive cytoplasm, although immunohistochemistry is typically not helpful in diagnosis. Electron microscopy may demonstrate relatively specific, zymogen like cytoplasmic granules that are electron dense, round - oval and membrane bound. The acinar tumor cells also have a well developed rough endoplasmic reticulum similar to normal salivary glands (see figure 5).
The differential diagnosis may include normal parotid gland, which has a lobular architecture with striated and interlobular ducts, as well as acinar cells. The follicular and papillary patterns may resemble thyroid carcinoma and the papillary pattern may resemble low grade salivary duct carcinoma (Am J Surg Pathol 2004;28:1040). Fine needle aspirations must be interpreted with caution, as they are often diagnosed as benign or nonneoplastic (Curr Opin Otolaryngol Head Neck Surg 2006;14:62).
Behavior is difficult to predict from histology. However, there is some general agreement on poor prognostic factors, many present in this case. They include pleomorphism (image 5), increased mitotic activity (image 6), vascular invasion (image 7) and clinical pain or fixation. Other poor prognostic factors are high stage, positive margins, tumor necrosis, stromal hyalinization, perineural invasion, large size and involvement of the deep lobe of the parotid gland.
Approximately 10 - 15% of acinic cell carcinomas metastasize, usually to local lymph nodes. Adequate excision is important, as it reduces the recurrence rate from 80 - 90% (with inadequate excision) to 10 - 30%. The surgeon can usually spare the facial nerve (Ear Nose Throat J 2005;84:597). Radiation therapy may be useful for positive surgical margins, advanced stage or high grade histology. Overall 5 year survival is 90%, the highest among parotid gland malignancies but late deaths also occur (Am J Otolaryngol 2005;26:39).
References: Ellis: Tumors of the Salivary Glands (Atlas of Tumor Pathology, 3rd Series, Vol 17), 1996