8 March 2006 - Case #39
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Mohanpal Dulai, William Beaumont Hospital, Royal Oak, Michigan, USA.
Case #39
Clinical history:
A 16 year old girl with no significant past medical history presented with amenorrhea for 5 months, headaches and new onset of seizures. Head MRI showed a 6.4 x 5.3 x 5.1 cm cystic, intensely enhancing mass in the anterior and central temporal lobe. There was moderate vasogenic edema with midline shift. The tumor was resected and consisted of tan-yellow, spongy tissue.
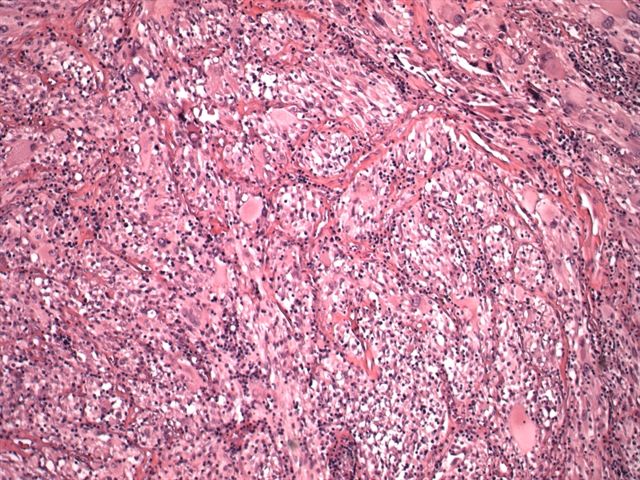
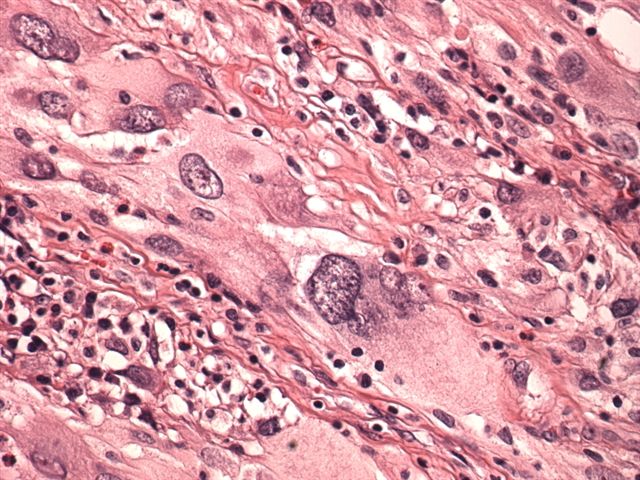
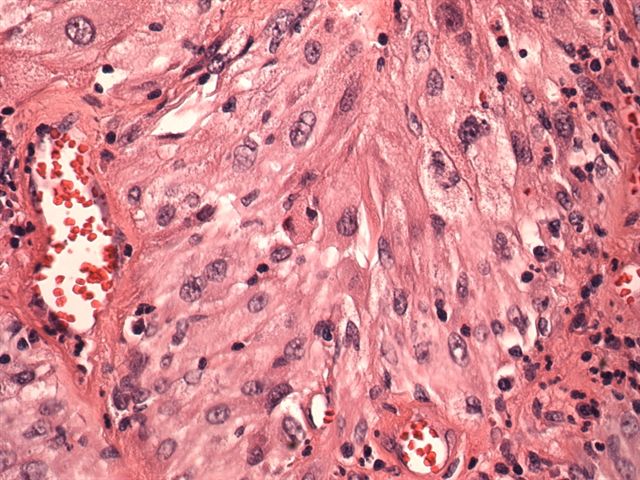
Microscopic images:
What is your diagnosis?
Diagnosis: Pleomorphic xanthoastrocytoma
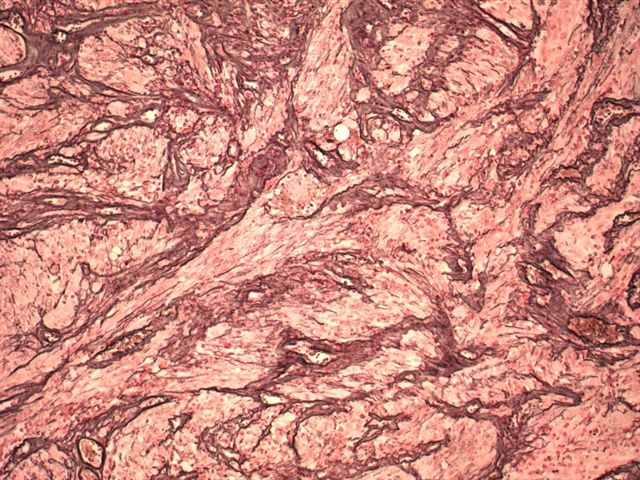
Stain image:
Discussion:
Pleomorphic xanthoastrocytoma is a rare, supratentorial tumor of children and young adults that often affects the temporal lobe and is associated with intractable seizures. Rare cases involve older adults. It was first described in 1979 and is graded as II of IV by the WHO (Cancer 1979;44:1839). Gross total resection usually eliminates the seizures, although 15% of tumors may progress to malignancy and long term follow up is recommended. Some authors consider it to be a developmental tumor that is associated with focal cortical dysplasia (J Neurooncol 2004;66:17). Radiologically, there is a large, well circumscribed mass with solid and cystic components or a cyst within a mural nodule.
Microscopically, the tumor contains markedly pleomorphic cells, including fibrillar astrocytes, which may contain foamy cytoplasm due to lipid. There are also large, bizarre, multinucleated giant cells and smaller spindle cells. Tumor cells may contain protein granular degeneration, similar to pilocytic astrocytoma. There is no necrosis and no mitotic figures, except in tumors with anaplastic features.
The tumor cells are almost universally immunoreactive for GFAP and S100, with prominent reticulin deposits also present. Variable immunostaining is present for neurofilament, synaptophysin and CD68. Tumor cells are negative for p53.
The diagnosis is usually not difficult. In cases with anaplastic features, the differential includes giant cell glioblastoma and malignant fibrous histiocytoma.
References: Am J Surg Pathol 2002;26:479 (immunostains), Arch Pathol Lab Med 2003;127:1187 (immunostaining compared to giant cell glioblastoma)
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Mohanpal Dulai, William Beaumont Hospital, Royal Oak, Michigan, USA.
Case #39
Clinical history:
A 16 year old girl with no significant past medical history presented with amenorrhea for 5 months, headaches and new onset of seizures. Head MRI showed a 6.4 x 5.3 x 5.1 cm cystic, intensely enhancing mass in the anterior and central temporal lobe. There was moderate vasogenic edema with midline shift. The tumor was resected and consisted of tan-yellow, spongy tissue.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Pleomorphic xanthoastrocytoma
Stain image:
Discussion:
Pleomorphic xanthoastrocytoma is a rare, supratentorial tumor of children and young adults that often affects the temporal lobe and is associated with intractable seizures. Rare cases involve older adults. It was first described in 1979 and is graded as II of IV by the WHO (Cancer 1979;44:1839). Gross total resection usually eliminates the seizures, although 15% of tumors may progress to malignancy and long term follow up is recommended. Some authors consider it to be a developmental tumor that is associated with focal cortical dysplasia (J Neurooncol 2004;66:17). Radiologically, there is a large, well circumscribed mass with solid and cystic components or a cyst within a mural nodule.
Microscopically, the tumor contains markedly pleomorphic cells, including fibrillar astrocytes, which may contain foamy cytoplasm due to lipid. There are also large, bizarre, multinucleated giant cells and smaller spindle cells. Tumor cells may contain protein granular degeneration, similar to pilocytic astrocytoma. There is no necrosis and no mitotic figures, except in tumors with anaplastic features.
The tumor cells are almost universally immunoreactive for GFAP and S100, with prominent reticulin deposits also present. Variable immunostaining is present for neurofilament, synaptophysin and CD68. Tumor cells are negative for p53.
The diagnosis is usually not difficult. In cases with anaplastic features, the differential includes giant cell glioblastoma and malignant fibrous histiocytoma.
References: Am J Surg Pathol 2002;26:479 (immunostains), Arch Pathol Lab Med 2003;127:1187 (immunostaining compared to giant cell glioblastoma)