1 March 2006 - Case #38
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Mohanpal Dulai, William Beaumont Hospital, Royal Oak, Michigan, USA.

Case #38
Clinical history:
A 54 year old Caucasian man with a history of von Hippel-Lindau disease, renal cell carcinoma, hypertension, polycythemia and multifocal hemangiomas presented with a headache of a few weeks duration. T1 weighted MRI images showed a cystic lesion with multiple enhancing mural nodules in the cerebellum. The lesion was resected and measured 1.2 cm with a red, hemorrhagic cut surface surrounded by spongy pink-tan tissue. No necrosis was identified.
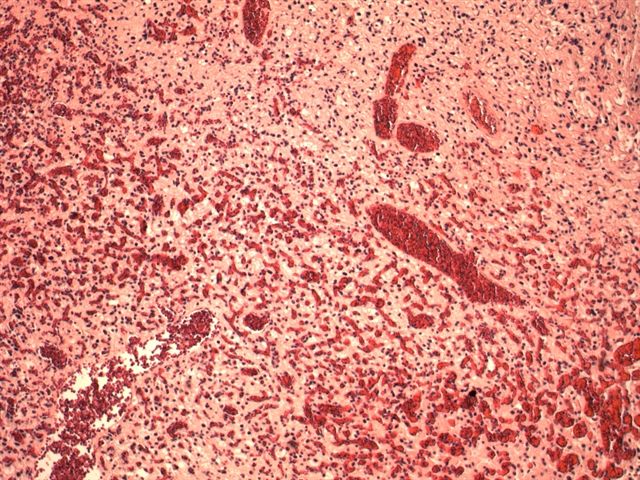
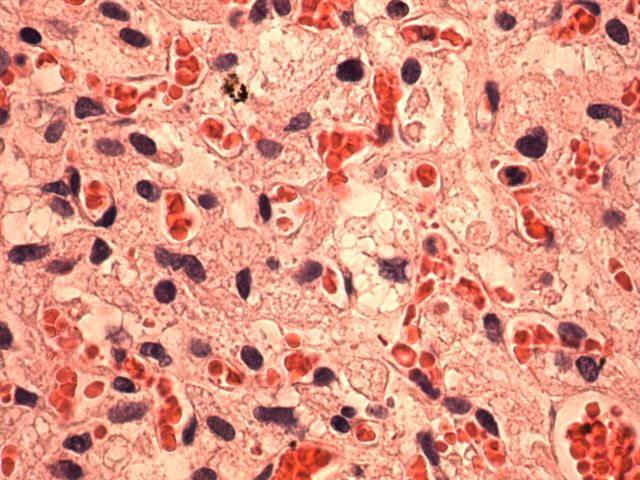
Microscopic images:
What is your diagnosis?
Diagnosis: Hemangioblastoma of the cerebellum
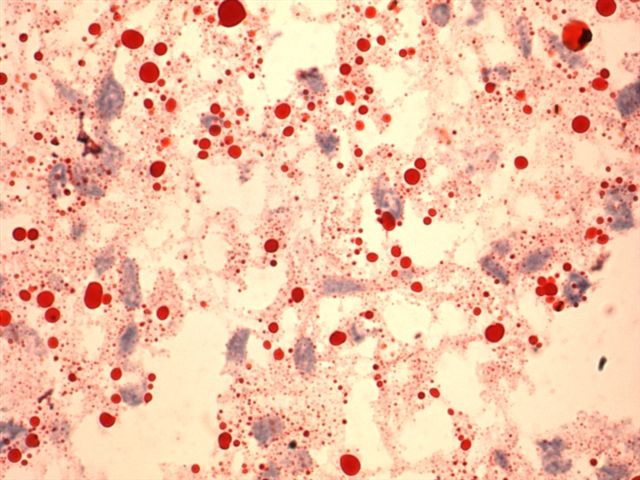
Stain image:
Discussion:
Hemangioblastoma is a slow growing and indolent tumor, which for CNS tumors, is graded I of IV (benign) by the World Health Organization (WHO). It represents 1 - 2% of intracranial tumors and is often in the cerebellum. Other sites include the spinal cord and meninges.
Hemangioblastoma is strongly associated with mutations of the von Hippel-Lindau (VHL) gene at 3p25-26, either as part of von Hippel-Lindau disease (25% of cases) or due to a sporadic mutation of the VHL gene. Loss of the VHL gene causes increased production of vascular endothelial growth factor, leading to richly vascular tumors such as hemangioblastoma, pheochromocytoma and clear cell type of renal cell carcinoma. Increased production of erythropoietin causes polycythemia.
Von Hippel-Lindau disease is a rare, autosomal dominant disorder characterized by hemangioblastomas of the cerebellum and retina, cysts of the liver and pancreas, pheochromocytoma and renal cell carcinoma. It presents at different ages and with varying manifestations, which often makes diagnosis difficult.
Grossly, hemangioblastomas are usually well circumscribed mural nodules within a large, fluid filled cyst. If a frozen section is requested, be sure to submit tissue from the mural nodule which contains the tumor, not from the cyst wall.
Histologically, the tumor is composed of a proliferation of capillaries of variable size, with large, neoplastic stromal cells containing pink to clear foamy cytoplasm with PAS+ vacuoles containing lipid. The nuclei are hyperchromatic but there no prominent pleomorphism or nucleoli or other atypical features. There is no necrosis and no / rare mitotic figures. There may be associated mast cells (Folia Neuropathol 1999;37:138). The cyst wall often has gliosis and Rosenthal fibers.
The differential diagnosis includes metastatic renal cell carcinoma, clear cell type (images of both tumors) and fibrillary astrocytoma. Renal clear cell carcinoma is also associated with von Hippel-Lindau disease and has prominent vascularity. However, unlike hemangioblastoma, the tumor cells often have prominent nucleoli and more marked pleomorphism and mitotic figures are present. Renal cell carcinoma is immunoreactive for cytokeratin and EMA but negative for NSE and inhibin. Hemangioblastomas have the opposite staining pattern (Mod Pathol 2005;18:788). Low grade astrocytomas exhibit gliosis and Rosenthal fibers and may stain for lipid at frozen section. However, they usually lack prominent vascularity and the morphologic features are different.
References: Medscape: Von Hippel-Lindau Disease [Accessed 27 March 2024], Genes and Disease: Von Hippel-Lindau Syndrome [Accessed 27 March 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Mohanpal Dulai, William Beaumont Hospital, Royal Oak, Michigan, USA.

Website news:
(1) IMPAC Medical Systems introduces PowerPath version 9.0 anatomic pathology information system. New features in version 9.0 include CAP Protocol Worksheet support with SNOMED CT resulting, enhanced GYN Cytology Reporting with HPV reflex testing, an advanced case search tool and laboratory worklist enhancements. In addition, IMPAC introduces new optional modules and interfaces that are compatible with version 9.0, including Immunohistochemistry Resulting, Enhanced Outreach Reporting, advanced histology barcoding and a cancer registry interface. These optional modules streamline resulting, increase report format options including color coded body site maps for GI and prostate specimens and facilitate specimen tracking to improve patient safety. Click here for more information.
Visit and follow our Blog to see recent updates to the website.
(1) IMPAC Medical Systems introduces PowerPath version 9.0 anatomic pathology information system. New features in version 9.0 include CAP Protocol Worksheet support with SNOMED CT resulting, enhanced GYN Cytology Reporting with HPV reflex testing, an advanced case search tool and laboratory worklist enhancements. In addition, IMPAC introduces new optional modules and interfaces that are compatible with version 9.0, including Immunohistochemistry Resulting, Enhanced Outreach Reporting, advanced histology barcoding and a cancer registry interface. These optional modules streamline resulting, increase report format options including color coded body site maps for GI and prostate specimens and facilitate specimen tracking to improve patient safety. Click here for more information.
Visit and follow our Blog to see recent updates to the website.
Case #38
Clinical history:
A 54 year old Caucasian man with a history of von Hippel-Lindau disease, renal cell carcinoma, hypertension, polycythemia and multifocal hemangiomas presented with a headache of a few weeks duration. T1 weighted MRI images showed a cystic lesion with multiple enhancing mural nodules in the cerebellum. The lesion was resected and measured 1.2 cm with a red, hemorrhagic cut surface surrounded by spongy pink-tan tissue. No necrosis was identified.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Hemangioblastoma of the cerebellum
Stain image:
Discussion:
Hemangioblastoma is a slow growing and indolent tumor, which for CNS tumors, is graded I of IV (benign) by the World Health Organization (WHO). It represents 1 - 2% of intracranial tumors and is often in the cerebellum. Other sites include the spinal cord and meninges.
Hemangioblastoma is strongly associated with mutations of the von Hippel-Lindau (VHL) gene at 3p25-26, either as part of von Hippel-Lindau disease (25% of cases) or due to a sporadic mutation of the VHL gene. Loss of the VHL gene causes increased production of vascular endothelial growth factor, leading to richly vascular tumors such as hemangioblastoma, pheochromocytoma and clear cell type of renal cell carcinoma. Increased production of erythropoietin causes polycythemia.
Von Hippel-Lindau disease is a rare, autosomal dominant disorder characterized by hemangioblastomas of the cerebellum and retina, cysts of the liver and pancreas, pheochromocytoma and renal cell carcinoma. It presents at different ages and with varying manifestations, which often makes diagnosis difficult.
Grossly, hemangioblastomas are usually well circumscribed mural nodules within a large, fluid filled cyst. If a frozen section is requested, be sure to submit tissue from the mural nodule which contains the tumor, not from the cyst wall.
Histologically, the tumor is composed of a proliferation of capillaries of variable size, with large, neoplastic stromal cells containing pink to clear foamy cytoplasm with PAS+ vacuoles containing lipid. The nuclei are hyperchromatic but there no prominent pleomorphism or nucleoli or other atypical features. There is no necrosis and no / rare mitotic figures. There may be associated mast cells (Folia Neuropathol 1999;37:138). The cyst wall often has gliosis and Rosenthal fibers.
The differential diagnosis includes metastatic renal cell carcinoma, clear cell type (images of both tumors) and fibrillary astrocytoma. Renal clear cell carcinoma is also associated with von Hippel-Lindau disease and has prominent vascularity. However, unlike hemangioblastoma, the tumor cells often have prominent nucleoli and more marked pleomorphism and mitotic figures are present. Renal cell carcinoma is immunoreactive for cytokeratin and EMA but negative for NSE and inhibin. Hemangioblastomas have the opposite staining pattern (Mod Pathol 2005;18:788). Low grade astrocytomas exhibit gliosis and Rosenthal fibers and may stain for lipid at frozen section. However, they usually lack prominent vascularity and the morphologic features are different.
References: Medscape: Von Hippel-Lindau Disease [Accessed 27 March 2024], Genes and Disease: Von Hippel-Lindau Syndrome [Accessed 27 March 2024]