7 December 2005 - Case #30
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Dylan Miller, Mayo Clinic, Rochester, Minnesota, USA.
Case #30
Clinical history:
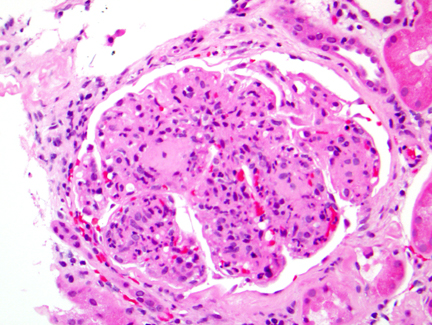
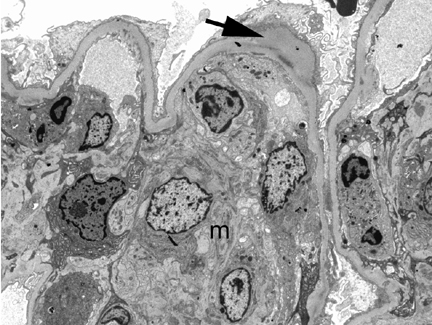
A 41 year old man with diabetes presented with renal failure 1 week after an upper respiratory infection. A renal biopsy was obtained and processed for H&E and electron microscopy.
Microscopic and electron microscopy images:
What is your diagnosis?
Diagnosis: Diabetic nodular glomerulosclerosis with superimposed postinfectious glomerulonephritis
Stains images:
Discussion:
This case features 2 distinct lesions consistent with the patient's history of diabetes and streptococcal infection (an ASO titer was elevated).
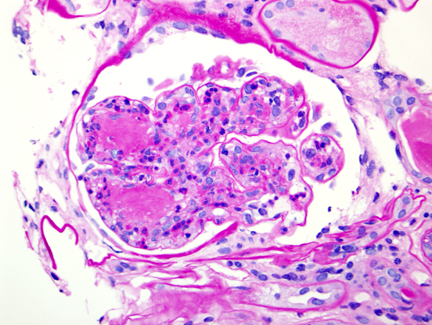
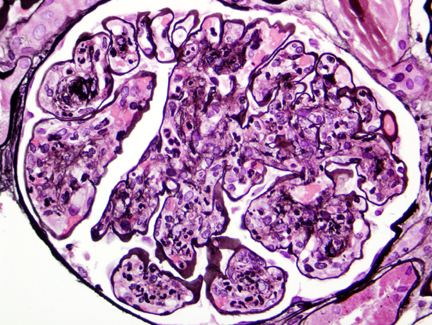
Patients with diabetes have numerous renal lesions, including nodular glomerulosclerosis, also called intercapillary glomerulosclerosis or Kimmelstiel-Wilson disease. These are ovoid, spherical, laminated hyaline masses in the periphery of the glomerulus that are PAS positive (additional image #1). They may eventually obliterate the glomerular tuft, causing end stage renal disease. They are relatively specific for diabetes but may also be found in membranoproliferative glomerulonephritis, light chain disease and amyloidosis.
Other microscopic diabetic renal lesions include (a) basement membrane thickening and increased mesangial matrix, in all patients; (b) diffuse glomerulosclerosis, identified by an increase in PAS+ mesangial matrix associated with basement membrane thickening, which eventually obliterates mesangial cells; (c) profound hyalinization of afferent arterioles (insudative lesion - intramural), which is specific for diabetes at this site (image); (d) organizing fibroepithelial crescents, associated with an aggressive clinical course; and (e) diffuse thickening of the tubular basement membrane, tubular atrophy and interstitial fibrosis.
Poststreptococcal glomerulonephritis is a diffuse type of endocapillary proliferative glomerulonephritis. It is also called postinfectious glomerulonephritis because similar histologic findings are seen with endemic malaria, toxoplasmosis, hepatitis B and C, HIV, varicella, spirochetes, staphylococci, meningococci and other bacteria. The deposition of immune complexes from antibodies against organisms elicits an acute inflammatory response and nephritic syndrome. Poststreptococcal disease is decreasing in the U.S., where post-Staphylococcal aureus infection is more frequent but it is common elsewhere. Histologically, the glomeruli are globally and diffusely enlarged and hypercellular due to neutrophils and macrophages and the proliferation of mesangial and endothelial cells. Capillary lumina are obstructed by swollen endothelial cells and inflammatory cells. Immunofluoresence shows a granular (lumpy bumpy) deposition of IgG, IgM and C3 in peripheral glomerular loops. EM shows subepithelial humps (finely granular, dome shaped, electron dense material, representing immune complex deposits) and the obliteration of epithelial cell foot processes.
A case of IgA dominant, poststaphylococcal glomerulonephritis complicating diabetic nephropathy has been reported (Hum Pathol 2003;34:1235).
References: Hum Pathol 1993;24:77 (pathogenesis of Kimmelstiel-Wilson nodule); also see our Kidney nontumor / medical renal chapter (click here)
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Dylan Miller, Mayo Clinic, Rochester, Minnesota, USA.
Case #30
Clinical history:
A 41 year old man with diabetes presented with renal failure 1 week after an upper respiratory infection. A renal biopsy was obtained and processed for H&E and electron microscopy.
Microscopic and electron microscopy images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Diabetic nodular glomerulosclerosis with superimposed postinfectious glomerulonephritis
Stains images:
Discussion:
This case features 2 distinct lesions consistent with the patient's history of diabetes and streptococcal infection (an ASO titer was elevated).
Patients with diabetes have numerous renal lesions, including nodular glomerulosclerosis, also called intercapillary glomerulosclerosis or Kimmelstiel-Wilson disease. These are ovoid, spherical, laminated hyaline masses in the periphery of the glomerulus that are PAS positive (additional image #1). They may eventually obliterate the glomerular tuft, causing end stage renal disease. They are relatively specific for diabetes but may also be found in membranoproliferative glomerulonephritis, light chain disease and amyloidosis.
Other microscopic diabetic renal lesions include (a) basement membrane thickening and increased mesangial matrix, in all patients; (b) diffuse glomerulosclerosis, identified by an increase in PAS+ mesangial matrix associated with basement membrane thickening, which eventually obliterates mesangial cells; (c) profound hyalinization of afferent arterioles (insudative lesion - intramural), which is specific for diabetes at this site (image); (d) organizing fibroepithelial crescents, associated with an aggressive clinical course; and (e) diffuse thickening of the tubular basement membrane, tubular atrophy and interstitial fibrosis.
Poststreptococcal glomerulonephritis is a diffuse type of endocapillary proliferative glomerulonephritis. It is also called postinfectious glomerulonephritis because similar histologic findings are seen with endemic malaria, toxoplasmosis, hepatitis B and C, HIV, varicella, spirochetes, staphylococci, meningococci and other bacteria. The deposition of immune complexes from antibodies against organisms elicits an acute inflammatory response and nephritic syndrome. Poststreptococcal disease is decreasing in the U.S., where post-Staphylococcal aureus infection is more frequent but it is common elsewhere. Histologically, the glomeruli are globally and diffusely enlarged and hypercellular due to neutrophils and macrophages and the proliferation of mesangial and endothelial cells. Capillary lumina are obstructed by swollen endothelial cells and inflammatory cells. Immunofluoresence shows a granular (lumpy bumpy) deposition of IgG, IgM and C3 in peripheral glomerular loops. EM shows subepithelial humps (finely granular, dome shaped, electron dense material, representing immune complex deposits) and the obliteration of epithelial cell foot processes.
A case of IgA dominant, poststaphylococcal glomerulonephritis complicating diabetic nephropathy has been reported (Hum Pathol 2003;34:1235).
References: Hum Pathol 1993;24:77 (pathogenesis of Kimmelstiel-Wilson nodule); also see our Kidney nontumor / medical renal chapter (click here)