All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Juan Segura Fonseca, Laboratorio de Patologa y Citologa Diagnstica S.A. (Costa Rica), for contributing this case and the discussion.
Orchard Pathology is an all-inclusive CP/AP diagnostic information system designed to accommodate the complex workflow and reporting of clinical, cytology, anatomic, and molecular testing.
Orchard Pathology is used for AP only or as a single system that includes clinical and molecularno more need for two separate systems. The shared database provides access to the patients history and enables the consolidation of clinical results to the pathology report. Unlike legacy text-based AP systems, Orchard Pathology stores report information in structured data fields that enhance EMR integration and simplify data mining for evaluations; correlation studies; quality assurance; and other management reports.
Visit us at
http://www.OrchardSoft.com.
(1) The topic search on the Home page now works for these chapters: Breast-nonmalignant, CD Markers CD1-CD49, Molecular Pathology and Skin-melanocytic tumors. We update the Topic search as we update each chapter. The Topic search looks for text within a topic's title (such as Langerhans cell histiocytosis or Medullary Carcinoma). In contrast, the Google Custom Search box searches our website for the occurrence of the search text anywhere on our website.
Visit and follow our Blog to see recent updates to the website.
Case #199
Clinical history:
This 44 year old woman was initially seen at our outpatient clinic in 2005 for a skin lump near the dorsum and ankle of the left foot. There was no history of trauma and a local excision was done, revealing irregular, non-encapsulated, subcutaneous fibrofatty tissue. The diagnosis was soft tissue angiolipoma. 4 years later, the lesion recurred (see images below).
Microscopic images:
What is your diagnosis?
Diagnosis: Hemosiderotic fibrohistiocytic lipomatous tumor
Discussion:
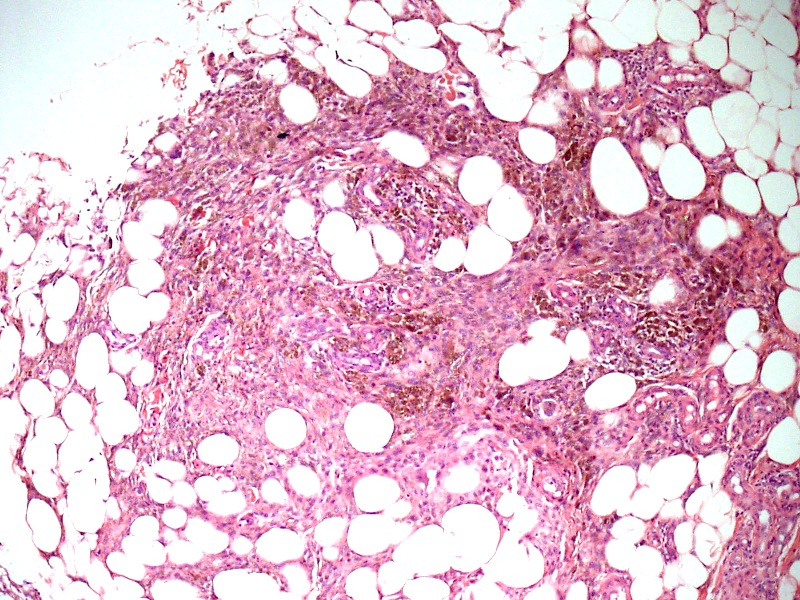
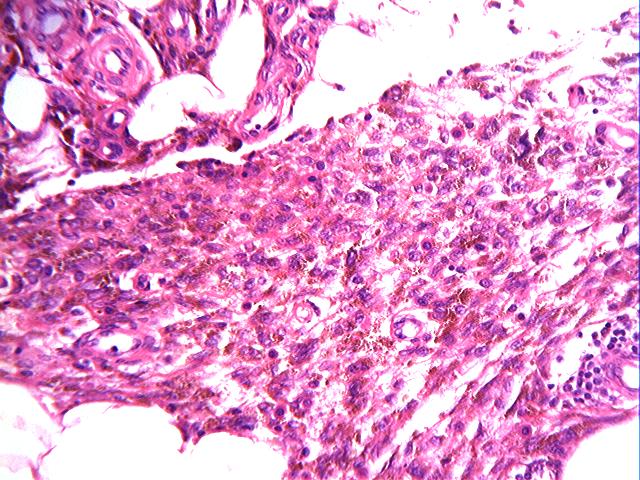
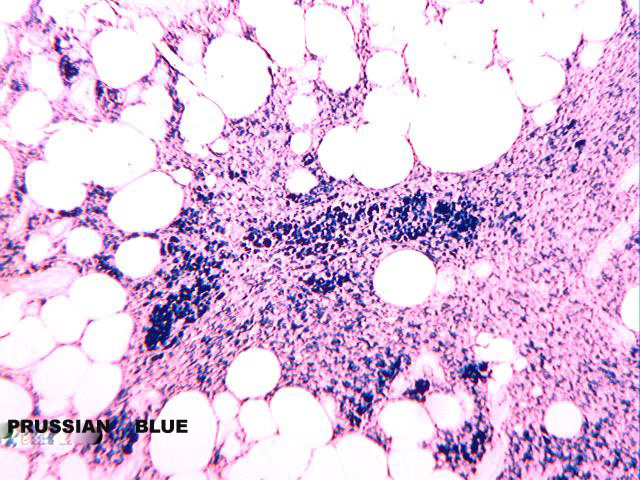
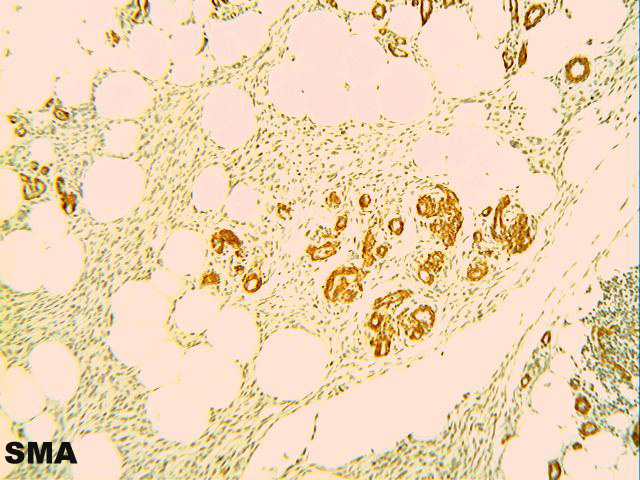
Microscopically, the lesion is characterized by 2 well defined tissue components, fatty tissue and spindle cells. The spindle cells are arranged in a dissecting pattern between adipocytic lobules and along the septae (figures 1 and 2). A minor focal inflammatory infiltrate is present (figure 3). Abundant hemosiderin pigment is present in the cytoplasm of the spindle cells as well in numerous macrophages located around blood vessels (figures 4 and 5). The pigment is positive for the Prussian blue iron stain (figure 7). Some small sized vessels are hyalinized (figure 6). An SMA immunostain highlights prominent vessels (figure 8) but does not stain the spindled cells, which are strongly positive for CD34 (figure 9).
Hemosiderotic fibrohistiocytic lipomatous tumor was first described by Marshall-Taylor and Fanburg-Smith (Mod Pathol 2000;13:1192). They described a peculiar soft tissue and subcutaneous lesion composed of CD34 positive fibroblastic cells, with a prominent vascularity and abundant hemosiderin within the cytoplasm of the spindle cells and many histiocytes. An associated lipomatous component was present. 8 patients were women and 2 were men. The mean age was 51 years. Almost all lesions were located in the foot, in the dorsum and around the ankle. Follow up in 8 patients revealed local recurrences in 4 (50%) over a 3 year period. No patients developed metastatic disease. There was a history of local trauma in 7 patients with ankle distortion and 2 of the women reported tight fitting, uncomfortable shoes.
Kazakov et al. reported 2 cases associated with venous stasis (Virchows Arch 2005;447:103). They hypothesized that the proliferation of the spindle fibroblastic cell component along with erythrocyte extravasation and formation of hemosiderin in the adipose tissue may simply represent an exaggerated tissue response to venous stasis. Browne and Fletcher reported 13 new cases and West et al emphasized the clinical location in the foot, the unique histopathological pattern and described the MRI characteristics (Histopathology 2006;48:453, Skeletal Radiol 2008;37:71). Recently, Wettach et al found a clonal reciprocal translocation between chromosomes 1 and 10, with a further chromosomal rearrangement in chromosomes 1 and 3, supporting a neoplastic and not reactive origin for this lesion (Cancer Genetics and Cytogenetics 2008;182:140).
Hemosiderotic fibrohistiocytic lipomatous tumor is rare. In a recent review of the literature, Oliveira et al found only 29 cases reported (Sao Paulo Med J 2009;127:174). All were biologically benign with no metastasis recorded. However, late local recurrences are frequent and pathologists should be aware of this lesion (Ann Chir Plast Esthet 2007;52:616).
This lesion may be related to or represent a precursor lesion of the pleomorphic hyalinizing angiectatic tumor of soft tissue, due to its vascular hyalinization (Pathol Int 2006;56:283, Am J Surg Pathol 2005;29:1256, Am J Surg Pathol 2004;28:1417).
The differential diagnosis includes several cutaneous and subcutaneous pigmented lesions of alleged fibrohistiocytic derivation: pigmented aneurysmal dermatofibroma (nodular, well localized storiform pattern), pigmented variant of dermatofibrosarcoma protuberans (called Bednar tumor, prominent cartwheel pattern, melanin pigment), Kaposi sarcoma plaque stage (RBC extravasation, PAS positive globules, some HHV8 nuclear positivity) and plexiform fibrous histiocytoma (mutinodular, storiform pattern, numerous multinucleated giant cells, scanty hemosiderin).