22 December 2010 - Case #193
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Mandolin Ziadie, Children's Medical Center of Dallas, Texas (USA) for contributing this case, with assistance from Dr. Barbara Hoffman and Dr. Lei Duan, University of Texas Southwestern Medical Center. This case was revised in July 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Case #193
Clinical history:
A 25 year old G4P2A1 woman presented at 36 weeks gestation with a positive maternal Quad screen (AFP, hCG, Estriol and inhibin A) for Down's syndrome but with normal amniocentesis. Placental thickening was noted on sonography. She delivered a normal appearing girl, 2254 grams (SGA / small for gestational age) with Apgars 9/9.
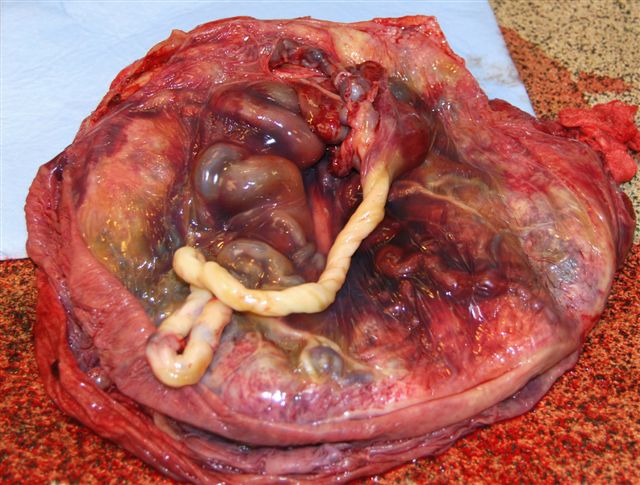
The gross examination shows a 1248 gram placenta, measuring 20.0 x 20.0 x 6.5 cm, with a 25.0 cm umbilical cord with velamentous insertion. The distal 15 cm of the cord is pale white and contains 3 vessels. At 10 cm from the disc, the cord is markedly dilated due to engorgement of the umbilical vein. No thrombi are present on sectioning. The fetal surface is purple-blue, smooth and shiny with tortuous, dilated chorionic plate vessels that measure up to 2 cm in diameter and taper off into numerous serpentine vessels that penetrate the disc. The maternal surface resembles an aggregate of pink-tan, tangled ropes interspersed by pale white cysts. The cut surface of the parenchyma is composed of dilated, worm-like vessels and small pale and occasionally blood filled cysts with minimal normal appearing intervening parenchyma. Near the point of cord insertion are multiple fleshy, firm soft tissue masses within the lumina of several small caliber vessels.
Gross images:
Microscopic images:
What is your diagnosis?
Diagnosis: Placental mesenchymal dysplasia with associated chorangiomatosis and features of fetal thrombotic vasculopathy
Discussion:
The microscopic images show (figures 1-12 are in rows 1-3 above):
Placental mesenchymal dysplasia is a rare placental vascular anomaly characterized by placentomegaly and grapelike vesicles resembling a partial molar pregnancy. Although its incidence is reported as 0.2%, it may be underdiagnosed and underreported, since it is relatively unknown to many pathologists (Congenit Anom (Kyoto) 2002;42:309, Arch Pathol Lab Med 2007;131:131, Surg Pathol Clin 2013;6:127, Arch Pathol Lab Med 2014;138:1247, Fetal Pediatr Pathol 2018;37:387).
Its underlying cause is unknown, although it is associated with Beckwith-Wiedemann syndrome (macroglossia, macrosomia [birth weight and length > 90th percentile], midline abdominal wall defects, ear creases or ear pits and neonatal hypoglycemia). Other possible etiologies include hypoxia and mosaicism. No association with fetal thrombotic vasculopathy has been described. Clinically, most patients present with an increased maternal AFP. There may be intrauterine growth restriction or fetal demise.
Gross features include a placenta large for gestational age (> 90th percentile), with aneurysmally dilated and tortuous chorionic plate vessels, that may show luminal thrombosis or rupture with hemorrhage. The parenchyma may have prominent stem villi and multiple grape-like cysts.
Microscopically, there are dilated thick walled vessels of the chorionic plate vessels with fibromuscular hyperplasia and variable fresh or organizing thrombi with possible luminal obliteration / thrombosis. The vessel walls show fibrinoid necrosis. There are parenchymal vascular malformations with dilated vessels with new / organizing thrombi. Stem villi are enlarged, up to 10 times normal. They have central cisterns that may be lined by lymphatic endothelium and are filled with gelatinous material (Placenta 2009;30:654). The stem villi have loose / myxoid stroma with abundant fibroblasts. Terminal villi may also show mesenchymal cell hypercellularity and stromal fibrosis. Vessels vary from chorangiomatous to being obliterated. Placental mesenchymal dysplasia is associated with loss of p57 in the stromal cells of dysplastic stem villi in almost all cases (Fetal Pediatr Pathol 2009;28:9).
The differential diagnosis includes a partial mole, but placental mesenchymal dysplasia has no trophoblastic proliferation, no stromal trophoblastic inclusions and no villous scalloping. Most cases are diploid. The differential diagnosis also includes spontaneous abortion with hydropic change, which may have vesicles, but they are usually small and focal, and are accompanied by degenerative changes.
~25% of cases of placental mesenchymal dysplasia are associated with Beckwith-Wiedemann syndrome. However, most phenotypically normal infants have no developmental problems.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Mandolin Ziadie, Children's Medical Center of Dallas, Texas (USA) for contributing this case, with assistance from Dr. Barbara Hoffman and Dr. Lei Duan, University of Texas Southwestern Medical Center. This case was revised in July 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Website news:
(1) Support PathologyOutlines.com by doing your holiday shopping at Amazon.com. Click here or on any Amazon banner on the left side of our Home Page to visit Amazon.com. Amazon not only sells books, but DVDs, electronics and clothing. By visiting Amazon via these links, they will send us 4-5% of the cost of all items you purchase (out of their profits), at no additional cost to you.
(2) We posted an article on our Management Page, Pathology Salaries and the Big Picture, by Mick Raich, Vachette Pathology.
Visit and follow our Blog to see recent updates to the website.
(1) Support PathologyOutlines.com by doing your holiday shopping at Amazon.com. Click here or on any Amazon banner on the left side of our Home Page to visit Amazon.com. Amazon not only sells books, but DVDs, electronics and clothing. By visiting Amazon via these links, they will send us 4-5% of the cost of all items you purchase (out of their profits), at no additional cost to you.
(2) We posted an article on our Management Page, Pathology Salaries and the Big Picture, by Mick Raich, Vachette Pathology.
Visit and follow our Blog to see recent updates to the website.
Case #193
Clinical history:
A 25 year old G4P2A1 woman presented at 36 weeks gestation with a positive maternal Quad screen (AFP, hCG, Estriol and inhibin A) for Down's syndrome but with normal amniocentesis. Placental thickening was noted on sonography. She delivered a normal appearing girl, 2254 grams (SGA / small for gestational age) with Apgars 9/9.
The gross examination shows a 1248 gram placenta, measuring 20.0 x 20.0 x 6.5 cm, with a 25.0 cm umbilical cord with velamentous insertion. The distal 15 cm of the cord is pale white and contains 3 vessels. At 10 cm from the disc, the cord is markedly dilated due to engorgement of the umbilical vein. No thrombi are present on sectioning. The fetal surface is purple-blue, smooth and shiny with tortuous, dilated chorionic plate vessels that measure up to 2 cm in diameter and taper off into numerous serpentine vessels that penetrate the disc. The maternal surface resembles an aggregate of pink-tan, tangled ropes interspersed by pale white cysts. The cut surface of the parenchyma is composed of dilated, worm-like vessels and small pale and occasionally blood filled cysts with minimal normal appearing intervening parenchyma. Near the point of cord insertion are multiple fleshy, firm soft tissue masses within the lumina of several small caliber vessels.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Placental mesenchymal dysplasia with associated chorangiomatosis and features of fetal thrombotic vasculopathy
Discussion:
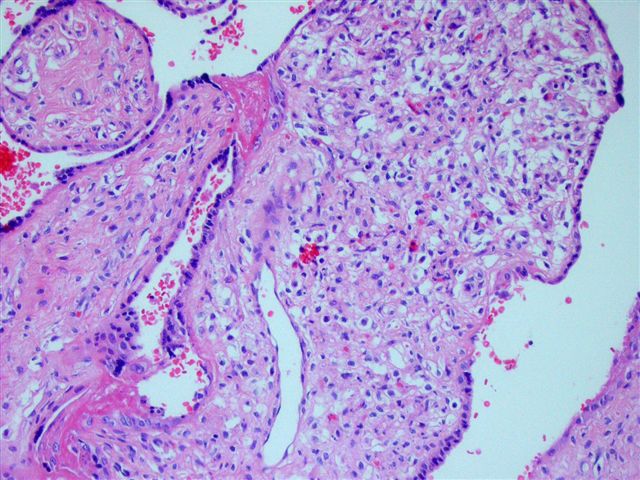
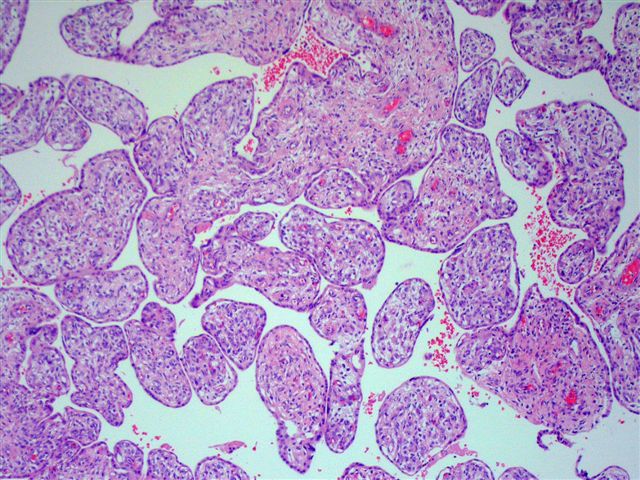
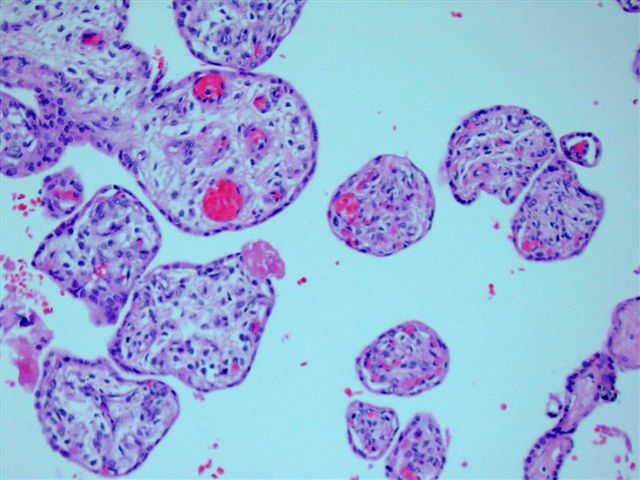
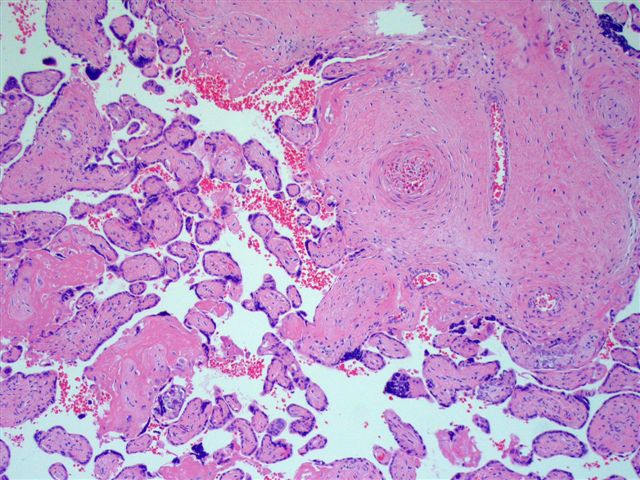
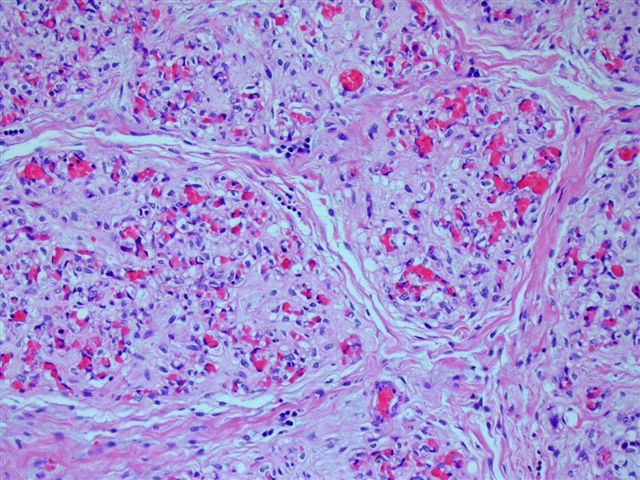
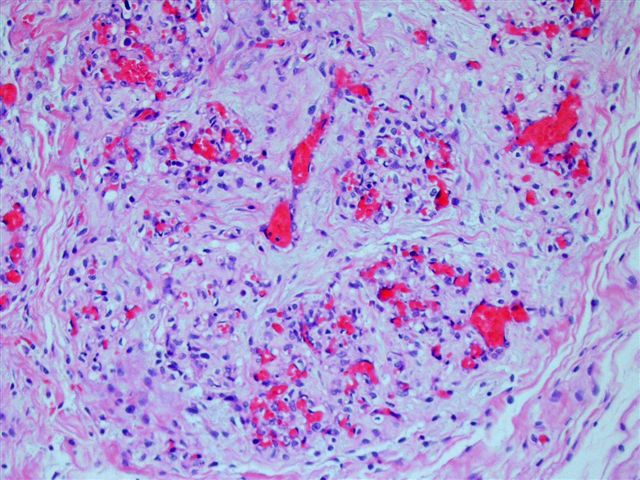
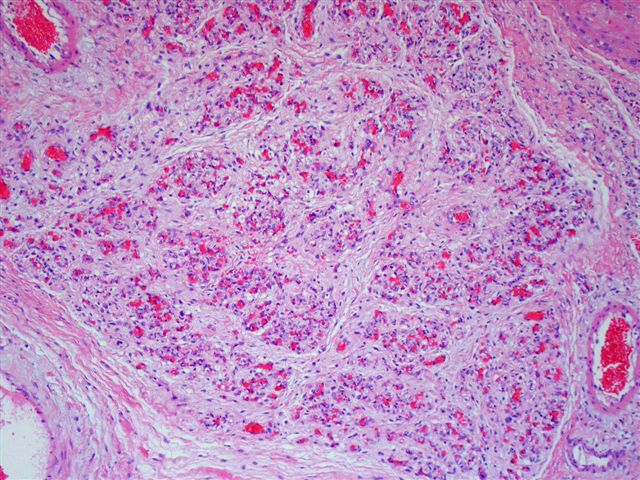
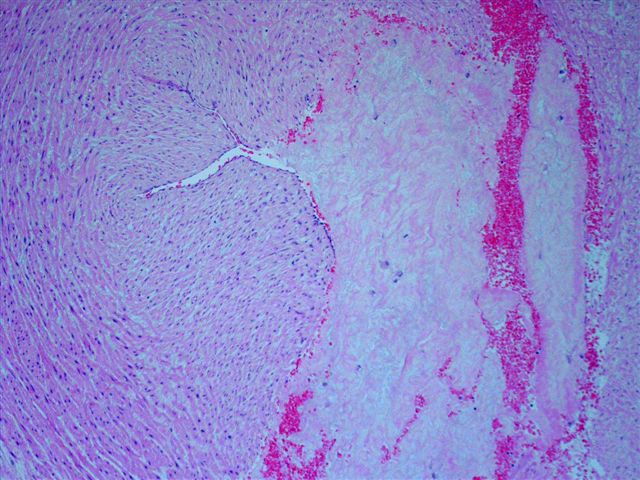
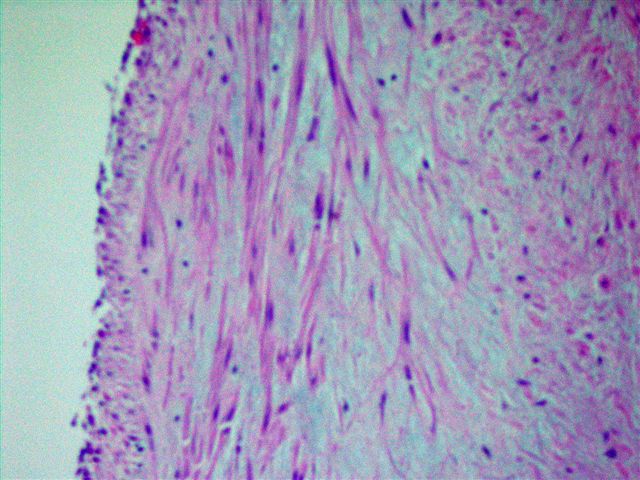
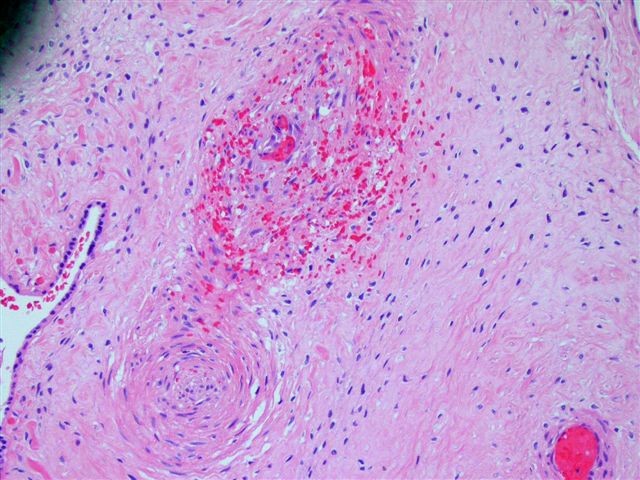
The microscopic images show (figures 1-12 are in rows 1-3 above):
- Figures 1 - 2: stem villous with central cistern and increased stromal mesenchymal cellularity
- Figures 3 - 4: tertiary villi with increased stromal cellularity and vascularity
- Figures 5, 6 and 12: vascular thrombi and avascular villi, consistent with fetal thrombotic vasculopathy
- Figures 7 - 9: localized chorangiomatosis with focal extramedullary hematopoiesis
- Figures 10 - 11: degenerative changes of umbilical vein smooth muscle
Placental mesenchymal dysplasia is a rare placental vascular anomaly characterized by placentomegaly and grapelike vesicles resembling a partial molar pregnancy. Although its incidence is reported as 0.2%, it may be underdiagnosed and underreported, since it is relatively unknown to many pathologists (Congenit Anom (Kyoto) 2002;42:309, Arch Pathol Lab Med 2007;131:131, Surg Pathol Clin 2013;6:127, Arch Pathol Lab Med 2014;138:1247, Fetal Pediatr Pathol 2018;37:387).
Its underlying cause is unknown, although it is associated with Beckwith-Wiedemann syndrome (macroglossia, macrosomia [birth weight and length > 90th percentile], midline abdominal wall defects, ear creases or ear pits and neonatal hypoglycemia). Other possible etiologies include hypoxia and mosaicism. No association with fetal thrombotic vasculopathy has been described. Clinically, most patients present with an increased maternal AFP. There may be intrauterine growth restriction or fetal demise.
Gross features include a placenta large for gestational age (> 90th percentile), with aneurysmally dilated and tortuous chorionic plate vessels, that may show luminal thrombosis or rupture with hemorrhage. The parenchyma may have prominent stem villi and multiple grape-like cysts.
Microscopically, there are dilated thick walled vessels of the chorionic plate vessels with fibromuscular hyperplasia and variable fresh or organizing thrombi with possible luminal obliteration / thrombosis. The vessel walls show fibrinoid necrosis. There are parenchymal vascular malformations with dilated vessels with new / organizing thrombi. Stem villi are enlarged, up to 10 times normal. They have central cisterns that may be lined by lymphatic endothelium and are filled with gelatinous material (Placenta 2009;30:654). The stem villi have loose / myxoid stroma with abundant fibroblasts. Terminal villi may also show mesenchymal cell hypercellularity and stromal fibrosis. Vessels vary from chorangiomatous to being obliterated. Placental mesenchymal dysplasia is associated with loss of p57 in the stromal cells of dysplastic stem villi in almost all cases (Fetal Pediatr Pathol 2009;28:9).
The differential diagnosis includes a partial mole, but placental mesenchymal dysplasia has no trophoblastic proliferation, no stromal trophoblastic inclusions and no villous scalloping. Most cases are diploid. The differential diagnosis also includes spontaneous abortion with hydropic change, which may have vesicles, but they are usually small and focal, and are accompanied by degenerative changes.
~25% of cases of placental mesenchymal dysplasia are associated with Beckwith-Wiedemann syndrome. However, most phenotypically normal infants have no developmental problems.