5 August 2010 - Case #183
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Arthur Somoza, University of Cincinnati Medical Center, Ohio (USA), for contributing this case.
Advertisement
Case #183
Clinical history:
An elderly patient had a tumor behind the left ear. 8 years ago, he had a parotid tumor excised, with an unknown diagnosis.
Gross images:
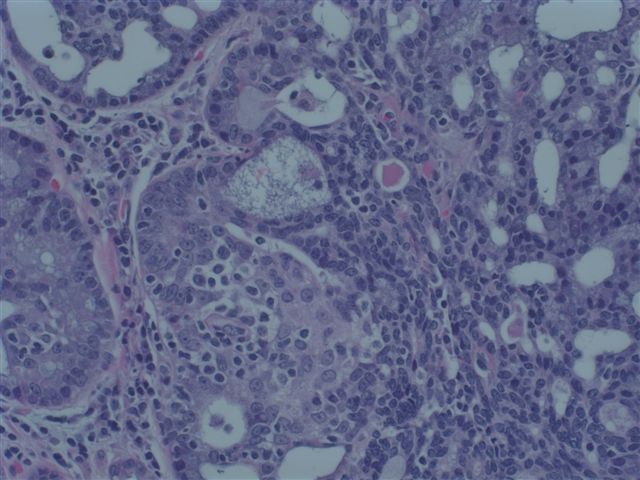
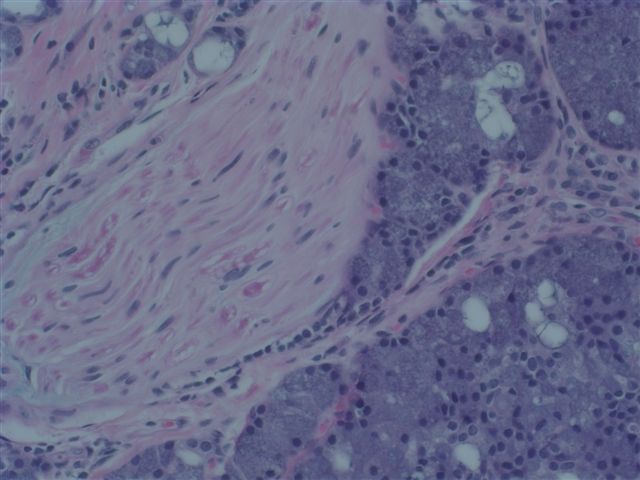
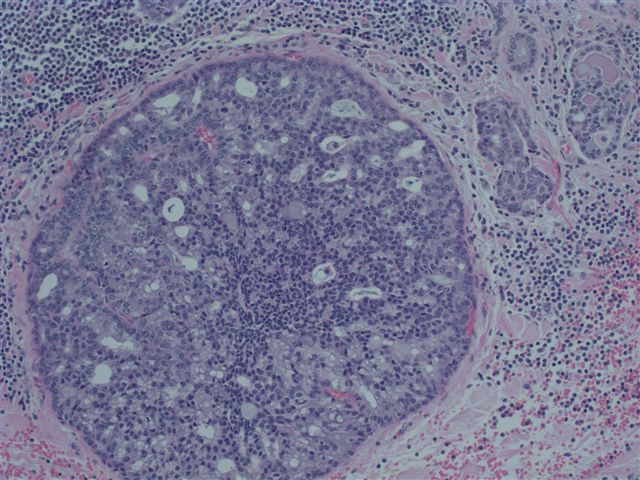
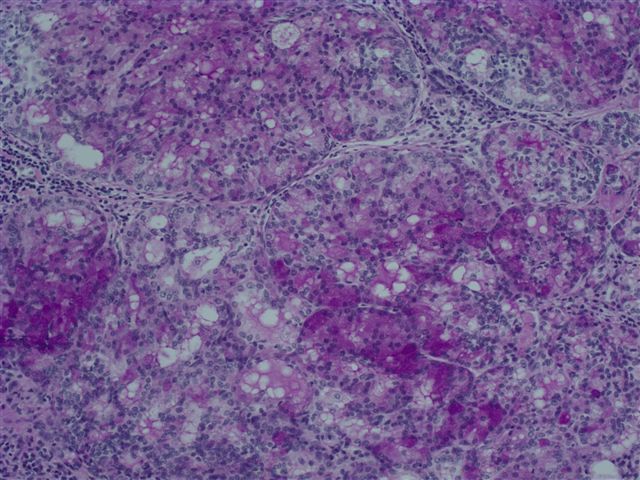
Microscopic images:
What is your diagnosis?
Diagnosis: Acinic cell carcinoma, metastatic
Discussion:
Review of the original slides showed similar histology as the current tumor.
Acinic cell carcinoma is defined as a salivary gland tumor with acinar cell differentiation. It represents up to 10% of salivary gland tumors. It often presents in patients under age 50 and is more common in women through age 50, with equal gender frequencies at older ages (Cancer Epidemiol Biomarkers Prev 2009;18:2899). It usually affects the parotid and minor salivary glands, as well as parotid lymph nodes. Clinically, it is less aggressive than other salivary gland tumors.
The tumors are typically encapsulated, 3 cm or less, tan-gray, solid or cystic. Only 3% are bilateral or multicentric. Most patients present with T1 or T2 disease.
Histologic patterns are variable, including solid, microcystic, papillary / cystic or follicular. The typical tumor cell resembles the salivary serous cell with basophilic granular cytoplasm, but there may also be clear cells containing glycogen or mucin, vacuolated cells or smaller glandular cells. Mitotic figures are rare. High grade transformation (previously called dedifferentiation) is rare and has polymorphic cells with a high mitotic rate arranged in glandular and solid growth patterns with comedonecrosis (Am J Surg Pathol 2009;33:1137). Other rarely reported features are neuroendocrine differentiation and psammoma bodies (Head Neck Pathol 2009;3:163, Acta Cytol 2009;53:440).
Tumor cells are immunoreactive for serous cell markers, including keratin, alpha-1-antichymotrypsin and alpha amylase. The cytoplasmic granules are PAS+ diastase resistant.
The differential diagnosis includes normal parotid tissue, which contains interlobular ducts and a lobular architecture, not found in acinar tumors.
Treatment consists of surgical excision with negative margins, with possible radiation therapy or lymph node dissection. Patients have a 5 year overall survival of 90% (Cancer 2009;115:2128). Overall, 10 - 15% develop metastases, usually to local lymph nodes. Recurrence occurs in 10 - 30%, often due to inadequate excision. Additional poor prognostic factors include extracapsular extension, facial nerve sacrifice, lymph node involvement at presentation and high grade features.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Arthur Somoza, University of Cincinnati Medical Center, Ohio (USA), for contributing this case.
The Genomic Health Oncotype DX Breast Cancer Assay provides early-stage ER-positive breast cancer patients with an individualized Recurrence Score result that assesses the benefit of chemotherapy and the likelihood of 10-year distant recurrence.
The Recurrence Score is calculated using RT-PCR technology to assess the expression of 21 genes in a patients FPET core biopsy or surgical excision sample. The assay is precise, accurate, and highly reproducible over a wide dynamic range, with a success rate of >97%. The assay is validated in 13 clinical studies involving more than 4000 patients.
For more information, please visit www.oncotypedx.com.
Oncotype DX and Recurrence
Score are registered trademarks of Genomic Health, Inc.
Website news:
(1) We added a feature to the Conferences page to quickly see the new postings, in reverse date posted. This feature was already present on the Jobs and Fellowship pages.
(2) We are redesigning our textbook pages so they load faster, by pulling the images directly from the server, instead of making them part of our file. Let us know if you notice any problems.
(3) We continue to update our 5000+ topics on a regular basis. If you are interested in reviewing a topic, please email us your CV and let us know what chapter and topics you are interested in reviewing.
Visit and follow our Blog to see recent updates to the website.
(1) We added a feature to the Conferences page to quickly see the new postings, in reverse date posted. This feature was already present on the Jobs and Fellowship pages.
(2) We are redesigning our textbook pages so they load faster, by pulling the images directly from the server, instead of making them part of our file. Let us know if you notice any problems.
(3) We continue to update our 5000+ topics on a regular basis. If you are interested in reviewing a topic, please email us your CV and let us know what chapter and topics you are interested in reviewing.
Visit and follow our Blog to see recent updates to the website.
Case #183
Clinical history:
An elderly patient had a tumor behind the left ear. 8 years ago, he had a parotid tumor excised, with an unknown diagnosis.
Gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Acinic cell carcinoma, metastatic
Discussion:
Review of the original slides showed similar histology as the current tumor.
Acinic cell carcinoma is defined as a salivary gland tumor with acinar cell differentiation. It represents up to 10% of salivary gland tumors. It often presents in patients under age 50 and is more common in women through age 50, with equal gender frequencies at older ages (Cancer Epidemiol Biomarkers Prev 2009;18:2899). It usually affects the parotid and minor salivary glands, as well as parotid lymph nodes. Clinically, it is less aggressive than other salivary gland tumors.
The tumors are typically encapsulated, 3 cm or less, tan-gray, solid or cystic. Only 3% are bilateral or multicentric. Most patients present with T1 or T2 disease.
Histologic patterns are variable, including solid, microcystic, papillary / cystic or follicular. The typical tumor cell resembles the salivary serous cell with basophilic granular cytoplasm, but there may also be clear cells containing glycogen or mucin, vacuolated cells or smaller glandular cells. Mitotic figures are rare. High grade transformation (previously called dedifferentiation) is rare and has polymorphic cells with a high mitotic rate arranged in glandular and solid growth patterns with comedonecrosis (Am J Surg Pathol 2009;33:1137). Other rarely reported features are neuroendocrine differentiation and psammoma bodies (Head Neck Pathol 2009;3:163, Acta Cytol 2009;53:440).
Tumor cells are immunoreactive for serous cell markers, including keratin, alpha-1-antichymotrypsin and alpha amylase. The cytoplasmic granules are PAS+ diastase resistant.
The differential diagnosis includes normal parotid tissue, which contains interlobular ducts and a lobular architecture, not found in acinar tumors.
Treatment consists of surgical excision with negative margins, with possible radiation therapy or lymph node dissection. Patients have a 5 year overall survival of 90% (Cancer 2009;115:2128). Overall, 10 - 15% develop metastases, usually to local lymph nodes. Recurrence occurs in 10 - 30%, often due to inadequate excision. Additional poor prognostic factors include extracapsular extension, facial nerve sacrifice, lymph node involvement at presentation and high grade features.