11 February 2010 – Case of the Week #169
This email is only sent to subscribers. To subscribe or unsubscribe to this or our other email lists, click here.
All cases are archived on our website. To view them sorted by number, diagnosis or category, visit our Home Page and click on the Case of the Week button on the left hand side.
Website News:
(1) We have updated the Staging sections for all chapters with information from
AJCC Cancer Staging Manual (7th ed)
(2) We have a new system to view your newsletter subscriptions.
Click here, then enter your email address on
our Subscribe page.
You will then be emailed a link that allows you to change your newsletter
preferences or your email address. Our newsletters are for 3 entities -
The Detroit College Promise (nonprofit that provides scholarships to Detroit students), PathologyOutlines.com (free online pathology textbook) and
DermatologyOutlines.com (free online dermatology textbook).
(3) We recently posted two new articles on our Management Page, Underpayment of Pathology Technical Component, by Mick Raich, Vachette Pathology and Payor Relationship Management Strategies and Trends: A Revenue Cycle Management Perspective, by Leigh Polk, PSA, LLC. The Management Page is accessed from the Home Page under Clinical Pathology chapters, or click here.
Thanks to Drs. Ashley Schneider, Julia Bridge, and David Wagner, University of Nebraska Medical Center, Omaha, Nebraska (USA) for contributing this case. To contribute a Case of the Week, follow the guidelines on our Case of the Week page.
Case of the Week #169
Clinical History
A 58 year old woman presented with an enlarging subfascial mass near the right scapula. An excisional biopsy was obtained.
The mass was negative for CD34, S100 and smooth muscle actin.
Micro images:
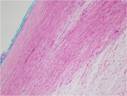
4x
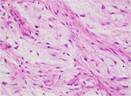
20x
40x
What is your diagnosis?
Diagnosis:
Low Grade Fibromyxoid Sarcoma
Discussion:
Molecular cytogenetics (FISH) on the
neoplasm revealed a t(7;16)(q32-34;p11) FUS-CREB3L2 fusion in 90% of examined
cells. This translocation is characteristic of a low grade fibromyxoid
sarcoma. The presence of a thick capsule is somewhat peculiar in this
case, as most low grade fibromyxoid sarcomas show microscopic invasion into
surrounding tissue. However, these lesions also tend to be well
circumscribed on gross examination.
Low grade fibromyxoid sarcomas is a rare, deceptively bland tumor first
described by Evans (Am
J Clin Pathol 1987;88:615). It is usually found in soft tissues of
adults (PathologyOutlines.com-Soft Tissue
Tumors part 1). The tumors are whorled with bland
spindled cells and areas of highly myxoid stroma. Nuclei are
elongated and nucleoli are small. There is no significant nuclear
pleomorphism or mitoses (Arch Pathol Lab Med 2006;130:1358). There may be
epithelioid areas or collagen rosettes. The tumor cells are immunoreactive
for vimentin, CD99, and bcl2, and negative for keratin, CD34 and
S100.
These tumors are closely related to, but morphologically distinct from the
hyalinizing spindle cell tumor with giant rosettes. Both neoplasms share
the same balanced translocation resulting in a FUS/CREB3L2 fusion gene.
Fine needle aspiration often results in an equivocal diagnosis (Cytopathology
2009;20:304).
The differential diagnosis includes:
Myxofibrosarcoma: more
myxoid and less fibrous, more nuclear pleomorphism and hyperchromatism, a
vascular network with prominent curvilinear and elongated capillaries is
present (Histopathology
2004;45:29).
Desmoid fibromatosis: no myxoid areas, fibrous cells are aligned straighter, cells appear more like reactive fibroblasts, distinct slit-like vessels are present; tumor has diffuse or occasionally focal nuclear beta catenin staining (AJSP 2005;29:653).
Neurofibroma: wavy nuclei, background of thick collagen bundles, S100+.
Fibrosarcoma-low grade fibroblastic type: no myxoid component, a diagnosis of exclusion (Histopathology 2006;49:152),
Treatment is complete excision. Despite their bland appearance, they may recur locally or rarely metastasize, but this appears to be less likely with aggressive surgery.
Additional references: Hum Pathol 2009;40:1586, Am J Clin Pathol 1987;88:615, Cytopathology 2009;20:304
Nat Pernick, M.D., President,
and Kara Hamilton, M.S., Associate Medical Editor
PathologyOutlines.com, Inc.
30100 Telegraph Road, Suite 408
Bingham Farms, Michigan (USA) 48025
Telephone: 248/646-0325
Email: NatPernick@Hotmail.com
Alternate email: NatPernick@gmail.com